 by Joe Monroe, MPAS, PA
by Joe Monroe, MPAS, PA
Mr. Monroe is a Fellow of the American Academy of Physician Assistants; is Founder, Past President, and Current Fellow of the Society of Dermatology Physician Assistants; and practices general and surgical dermatology in Tulsa, Oklahoma.
J Clin Aesthet Dermatol. 2020;13(9 Suppl):S29–S34
FUNDING: No funding was provided for the preparation of this article.
DISCLOSURES: The author has no conflicts of interest relevant to the content of this article.
Contact dermatitis caused by the sap of plants from the Anacardiaceae family, including poison ivy, oak, and sumac, is among the most common skin conditions in the United States. The author reports the case of a 50-year-old man who presented with numerous vesicles and flaccid bullae on erythematous bases on his right volar wrist; smaller areas of vesiculation on his trunk and legs, several of which displayed a linear configuration; and erythema and swelling on and around his penis. The patient was diagnosed with Toxicodendron contact dermatitis caused by exposure to poison ivy. The author describes symptoms, assessment methods, and differential diagnoses, as well as provides a brief review of pathologic and etiologic factors, epidemiology, and treatment approaches for cutaneous dermatitis caused by contact with poison ivy and related plants. The author also provides an brief history, recommended therapies, and notable physical characteristics of poison ivy, with the final takeaway point—Clinicians should educate their patients on how to identify, and, thus, avoid, contact with these highly irritating plants.
KEYWORDS: Toxicodendron, contact dermatitis, poison ivy, poison oak, sumac, Rhus, delayed hypersensitivity
Toxicodendron contact dermatitis (TCD) is a highly pruritic papulovesicular eruption that represents a Type-IV delayed hypersensitivity reaction triggered by contact with the sap of plants from the Anacardiaceae family, which includes poison ivy (the most common), oak, and sumac.1 These and similar plants are found in temperate climates around the world, including North America. Sap from the injured leaves, stems, and berries of these plants contain an oily resin called urushiol, to which 85 to 90 percent of adults are allergic. Exposure to urushiol can result in an intensely pruritic and potentially blistery rash that can persist for weeks regardless of treatment, and each additional exposure to urushiol can cause increasingly severe skin reactions. The respiratory system can also be affected by aerosolized allergens, if the smoke of the burning plant is inhaled, bringing on reactive airway symptoms and even anaphylaxis in some patients. Currently available treatments for TCD are unsatisfactory, often only slightly easing the symptoms while the condition slowly fades on its own. Treatment becomes even more difficult due to erroneous beliefs, some centuries old, that persist to this day.2,3 Already ubiquitous, poison ivy and related plants have become increasingly widespread and toxic due environmental factors, such as rising atmostpheric CO2 levels, off of which these plants thrive, caused by global warming.4
This article describes the case of a middle-aged man who developed severe TCD following exposure to poison ivy. Symptoms, patient assessment, diffential diagnoses, and treatment options are discussed. The history of poison ivy classification, related misconceptions, and identifying characteristics of the plant are also reviewed.
CASE REPORT
Patient presentation and history. A 50-year-old man presented to the dermatology clinic with frank, fluid-filled, pruritic blisters on his forearms, hands, wrists, trunk, and legs. The patient reported that, two weeks prior to presentation, he had cleared dead weeds, vines, and other debris from along the fence in his backyard, bunching them together by hand and carrying them to a nearby trash container. Within 48 hours, itchy blisters began forming on his arms, hands, and wrists, and within a week, had spread to his trunk and legs. The patient self-treated using over-the-counter topical calamine lotion and oral diphenhydramine 50mg twice daily but did not find relief. Due to the severity of pruritus, the patient sought care at a local urgent care clinic and was diagnosed with dermatitis with secondary infection. The patient was prescribed a pack of short-term, low-dose prednisolone and trimethoprim-sulfa double-strength tablets to be taken twice a day for a week. According to the patient, neither treatment offered any relief. At this point, the urgent care provider referred the patient to the local dermatology clinic.
Dermatology examination. In the dermatology clinic, the patient appeared anxious but was afebrile and in no acute distress. The patient had no history of atopy or immune suppression, and he denied any fever, joint pain, or malaise. He pointed to the involved areas on his body where vesicles and flaccid bullae on erythematous bases could be seen. Dermatitis was most severe on the volar wrist (Figure 1), but several other smaller areas of vesiculation could be seen on the trunk and legs, several of which displayed a linear configuration (Figure 2). His penis and surrounding areas were erythematous and swollen. None of the areas were tender to touch nor especially warm, and there was no palpable adenopathy in the area. There were no signs of infection (e.g., no pain, fever, purulence, or regional adenopathy).4


Any number of contactants could have caused a similar reaction to that observed in this patient, including other common plants. For example, Virginia Creeper, a very common climbing vine often seen near poison ivy, can trigger a similar rash due to oxalate crystals in its leaves and stems;5,6 however, the rash caused by VIrginia Creeper typically is less severe than than that caused by poison ivy, and it affects a relatively small percentage of the population. Given the patient’s previous history of poison ivy exposure, combined with his recent spate of yardwork, poison ivy was the most obvious suspect, and this case was judged to be consistent with a classic poison ivy rash, also known as TCD. Unbeknownst to the patient, who purposely waited until the fall weather had killed off the poison ivy before attempting to clear it from his yard, poison ivy can cause such eruptions long after the plant has died.
Case treatment. The patient was prescribed triamcinolone 0.5% cream for twice daily application, along with an intramuscular injection of triamcinolone 40mg, and hydroxyzine 25mg to be taken once daily at bedtime to help the patient sleep. The patient was also advised to obtain over-the-counter (OTC) aluminum acetate powder to be mixed with tap water, according to package directions, creating a topical solution that could be applied to affected blistery areas twice a day to help dry the blisters and reduce irritation. Extensive education was provided to the patient regarding the benign, noncontagious, and self-limited nature of the condition, and he was cautioned to avoid future contact with poison ivy due to the likelihood that his reaction to the plant would increase in severity with each additional exposure.7 The patient was seen in weekly intervals, and within two weeks he was almost totally clear.
DISCUSSION
History. Poison ivy is neither poisonous nor a true member of the Ivy family (Hedera). Instead, it is a member of the Anacardiaceae family, which also includes pistachios, cashews, and mangoes. All members of the Anacardiaceae family contain various forms of pentadecylcatechols within their sap, which is collectively termed urushiol, an oleoresin released from the injured leaves, stems, vines, or berries of these plants.7
The word urushiol is derived from the Japanese word urushi, which is the name of the black lacquer harvested from Japanese lacquer trees and used for decorative purposes in a process first documented in Japan thousands of years ago. Interestingly, a 20th century Japanese scientist, Rikou Mazima, was the first to identify and name urushiol, the allergen common to the entire Toxicodendron family, of which poison ivy, oak, and sumac are members.8
The first known reference to poison ivy dates back to 7th century China.9 In 1624, however, John Smith, an English explorer best known for his role in establishing the first permanent English colony in America, published the first written account of poison ivy, which he based on the unpublished writings of Nathaniel Butler, governor of Bermuda at that time. Later, in 1784, Philadelphia botanist William Bartram brought poison ivy to the Old World, along with 220 other American trees and plants, and the effects of poison ivy and related plants soon became widely known in Europe.8
Poison ivy’s original classification, Toxicodendron radicans (T. radicans), was first established by the French botanist Joseph Pitton de Tournefort in the 17th century. Later, Carl Linnaeus, considered the “Father of Taxonomy,” classified poison ivy, poison oak, and poison sumac under the Rhus genus in 1737.8 However, by the 18th century, 27 species of Rhus had been identified, with numerous variations, creating the need to better clarify the taxonomic designations of plants falling into the Rhus genus. Thus, the genus Toxicodendron, which means “poison tree,” was reprised for what we know today as poison ivy, poison oak, and poison sumac, with radicans and rydbergii being the most common species. Poison oak (T. diversilobum) is more common in western United States, and poison sumac (T. vernix) is primarily confined to marshy areas of eastearn and southeastern United States, but numerous types of Toxicodendron plants can be found in temperate climates all over the world.7
Symptoms. Approximately 50 to 75 percent of the US adult population is clinically sensitive to poison ivy, oak, and sumac.10 The cutaneous reaction usually begins 12 to 72 hours after contact with the plant, manifesting with intense itching that is often accompanied by the formation of vesicles or bullae, which tend to present in linear configurations following the pattern of contact made by plant’s leaves, berries, stems, or vines (Figure 2).11,12 The combination of itching, the linear configuration of the lesions, and a history of recent exposure to the plant is essentially pathognomic. The rash and related symptoms can last a month or more, with or without treatment.
Differential diagnoses. In addition to other contactants, the list of differential diagnoses for blistering diseases, in general, is lengthy and includes pemphigus, bullous pemphigoid, and a wide variety of other immune-mediated disorders. Adverse reactions to drugs can present with similar but more widespread involvement. Herpes zoster is a possibility, but typically involves a unilateral, dermatomal distribution, with complaints of pain in addition to itching and burning.1,9
Treatment. The patient in this case report was one of approximately 500,000 cases of TCD reported each year in the United States.17 The patient’s treatment with oral prednisolone prior to being seen by the dermatology clinic was typical but did not relieve his symptoms, nor did the calamine lotion or oral diphenhydramine.1,13
Key to preventing TCD is the ability to recognize these plants and, thus, avoid contact with them. Failing that, thoroughly washing skin that has come into contact with the plant using large amounts of water should be done as soon as possible after exposure (ideally within 20 minutes).2,9 Some reports state that certain types of soap can spread of the plant’s oils on the skin and should only be used after thoroughly rinsing the area with water.2 Once the immune system is triggered by the penetration of the oily resin, however, no amount of washing can help.2
Over-the-counter treatments for symptoms of poison ivy include external analgesics, such as benzocaine, pramoxine, and benzyl alcohol; protectants, such as zinc acetate, zinc carbonate, zinc oxide, calamine (a combination of zinc oxide, ferric oxide, mixed with phenol and calcium hydroxide), baking soda, and colloidal oatmeal; aluminum acetate (an astringent); hydrocortisone; Burow solution (an aqueous solution of aluminium triacetate); and oral diphenhydramine.1,9 It is not advised to apply topical antihistamines (e.g., topical diphenhydramine) to the rash due to its potential to worsen the symptoms.7 Unfortunately, while many of these OTC treatments might assist in drying out the weeping, oozing blisters associated with poison ivy, they often do not provide sufficient relief, especially in severe cases.1,9,13
While there is no entirely satisfactory treatment for TCD other than the “tincture of time,” longer-course glucocorticoid therapy, such as triamcinolone or prednisone, has been shown to be effective in relieving symptoms associated with TCD.8 Short courses of low-dose methylprednisolone (so-called “dose paks”) are too brief and too weak to offer effective relief. Glucocorticoids should be administered using a 2- to 3-week taper starting with 60mg daily (preferably taken in the morning with food to avoid gastritis) for five days that is reduced to 40mg daily for five days and then down to 20mg daily for five days.9,8 Contraindications for glucocorticoids include concurrent infection, peptic ulcer disease, poorly controlled hypertension, congestive heart failure, and diabetes.9 Dementia can also be made worse with systemic steroids (so-called “steroid psychosis”).9 Less serious side effects of systemic glucocorticoids include an increase in appetite, retention of fluid (edema), irritability, and insomnia. Adrenal suppression associated with prolonged systemic steroid use is rarely a problem when using a 2- to 3-week course of glucocorticoid therapy for poison ivy.9
In addition to oral glucocorticoid therapy, a one-time intramuscular injection of a glucocorticoid (40 to 60mg) works quickly and may be offered in severe cases of poison ivy, with the same precautions as those for the oral formulations. The addition of a bedtime dose of a effectively sedating antihistamine, such as hydroxyzine 25 to 50mg, and application of aluminum acetate compresses (Burow solution), can also be helpful. The use of topical steroid creams or sprays, such as betamethasone or triamcinolone, can reduce itching, but application must be limited to nonintertriginous areas and should only be used for a short period of time due to the risk of skin atrophy.1
Misconceptions. TCD not only can cause substantial physical discomfort for the patient, but may also cause psycho-social discomfort due to the common misconception that poison ivy is actually poisonous and its physical effects on affected skin are contagious, such that the affected patient might be sequestered in his or her own household. We now know that once the oily resin has been removed from the skin, TCD cannot be transmitted from one person to another person, or from one area of the body to another area, though contact with residual urushiol on clothing, tools, and pets can trigger new eruptions.1,7,14,15
Prevalence. Prevalance of poison ivy has doubled since 1960, and its potency is rapidly increasing, making this rash a common complaint in dermatology offices. Several factors contribute to this increase in prevalence:
Increased development of land in which margins are delineated by fences, electric lines, trees, and bushes make excellent habitats for poison ivy and the birds and other animals that consume its berries.
Birds are avid consumers of the plant’s berries, which are passed through the digestive tract and excreted onto the ground, where they take root.
Longer, warmer growing seasons brought on by climate change contribute to the growth and spread of the plant.
The increased atmospheric CO2 level caused by global warming not only promotes the growth of these plants (poison ivy and related plants thrive off of CO2), but also cause the plants to produce more potent forms of urushiol. The number of these plants is expected to double again when atmospheric CO2 levels, now at 410ppm, the highest in three million years, reach 560ppm.3,16
TCD places a financial burden on our economy and utilizes substantial healthcare resources. For example, outdoor occupations related to agriculture, forestry, and firefighting are at high risk of exposure to poison ivy, and when affected, these workers incur significant monetary expense for worker disability and medical treatments.TCD is responsible for 10 percent of the total US Forest Services lost work time due to injuries.17
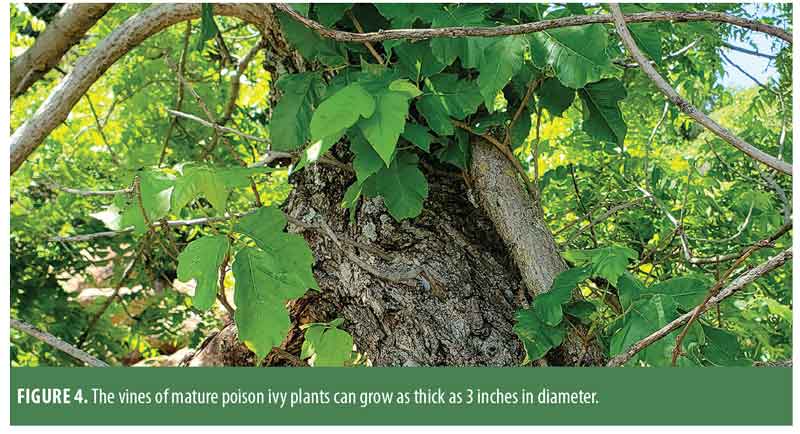
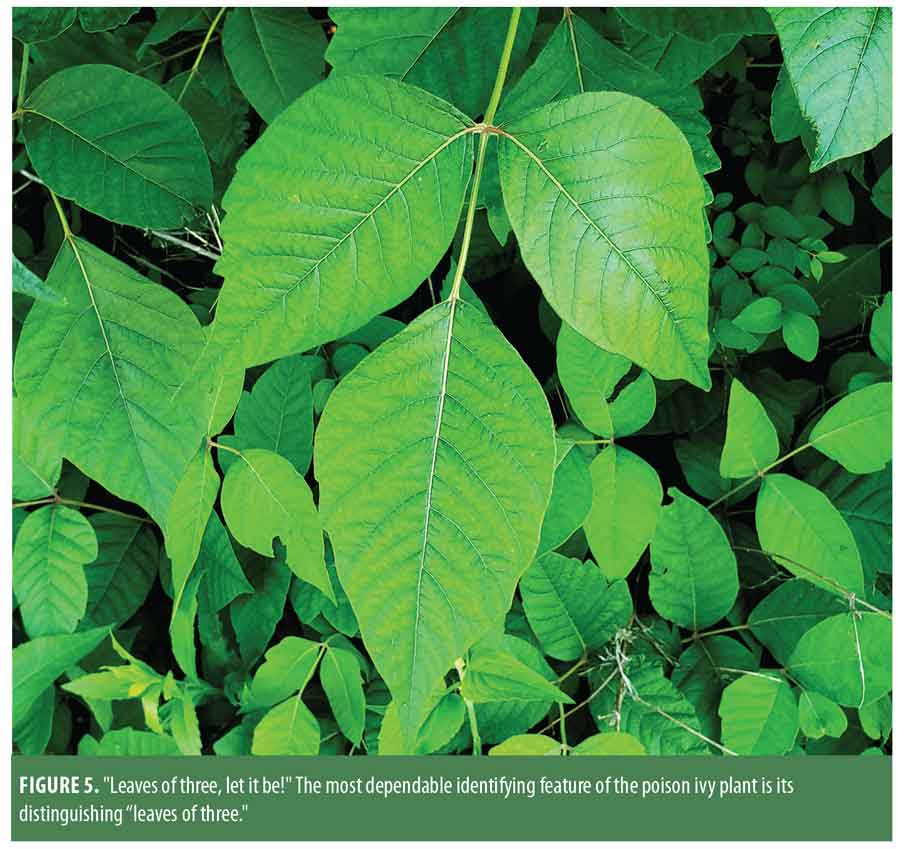
Indentifying features. A key factor in managing TCD relies first on educating the public on how common poison ivy is and how to identify it (and thus avoid it). The latter is can be difficult because Toxicodendron plants display a wide variety of features. For example, a Toxicodendron plant can present as a small shrub, as a low-lying vine, or a distinctive vine that attaches itself to the base of a tree, climbing to astonishing heights. When fully mature, the poison ivy vine is covered by tiny, rough, “hairy” rootlets (hence the old saying “Hairy vine, no friend of mine!”), which help the plant attach itself to large trees growing near water sources (Figure 3). These vines can grow up to three inches in diameter (Figure 4). From these mature vines, solitary stems extend outward an inch or two, displaying three distinct leaves at the terminus. The nonserrated, shiny leaves often display a notch or two on their periphery (sometimes referred to as “thumbs”). The young blackberry has similarly shaped leaves; however, it can be distinguished by the presence of thorns, which poison ivy plants lack. The lack of serrated leaf edges helps to distinguish poison ivy from Virginia creeper (Parthenocissus quinquefolia), which is often found near or mixed in with poison ivy plants. Virginia creeper displays five serrated elliptical leaves emanating from a single smooth stem.5

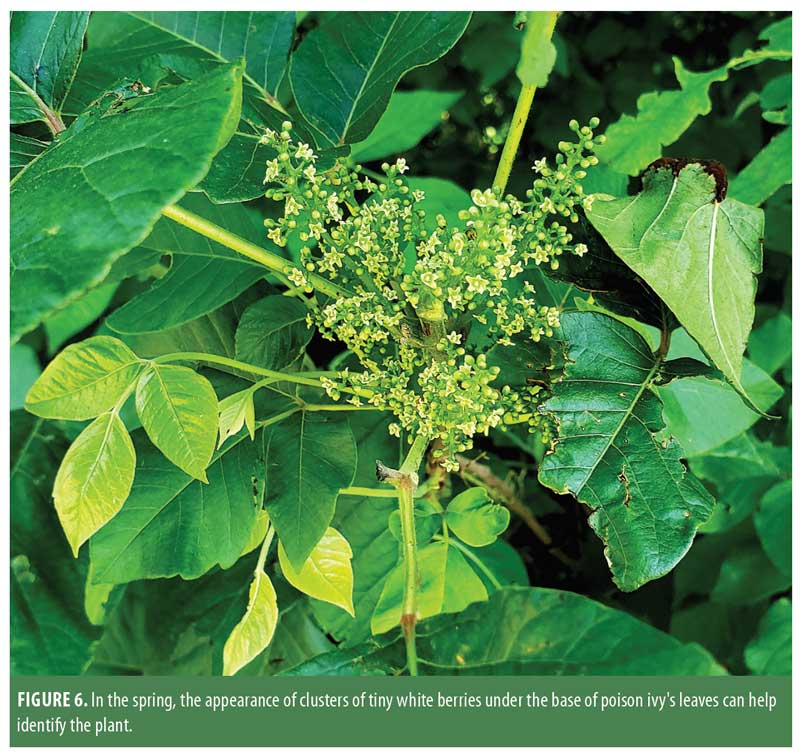
The most dependable identifying feature of the poison ivy plant is the legendary “leaves of three” (inspiring the saying “Leaves of three, let it be!”) (Figure 5). The leaves can vary in length from 1 to 8 inches4 and are a shiny green when they first appear, turning a bright red in the fall. Other identifying features include clusters of tiny white “berries” under the base of the leaves, which first appear in the spring (Figure 6). Otherwise, the appearance of the plant can vary a great deal depending on environmental factors, such as water, predation by insects, and light exposure.10
SUMMARY
Toxicodendron plants, including poison ivy, oak, and sumac, are common throughout the US. Global warming and land development are causing the prevalence and potency of these plants to increase rapidly. The rash caused by contact with the leaves, stems, or berries of these plants is highly pruritic, can last for weeks, and can have a substantially negative impact on a patient’s quality of life, including loss of sleep and missed work days. Currently, the only effective treatment for TCD is a 2- to 3-week course of a systemic glucocorticoid, which is primarily used to alleviate the severe itching associated with the rash. Some OTC topical formulations may offer limited itch relief and assist in drying out the blistery rash. Patient education on how to recognize, and, thus, avoid contact with Toxicodendron plants is a key component to preventing TCD.
REFERENCES
- Stephanides SL, Miller MA. Toxicodendron poisoning treatment and management. Last updated 13 Aug 2020. Medscape site. https://emedicine.medscape.com/article/817671-treatment#d11. Accessed 22 Sep 2020
- Lofgran T, Mahabal G. Toxicodendron toxicity. StatPearls. Last Update: April 19, 2020. Treasure Island, FL: StatPearls Publishing; 2020. https://www.ncbi.nlm.nih.gov/books/NBK557866/. Accessed 17 Sep 2020.
- Crawford G, Elston D. Botanical dermatology. Medscape site. http://misc.medscape.com/pi/android/medscapeapp/html/A1090097-business.html. Accessed September 4, 2020.
- Mohan J, Ziska L, Clark JS. Biomass and toxicity responses of poison ivy to CO2. Proc Natl Acad Sci USA. 2006;103: 9086–9089.
- Petrides GA. A Field Guide to Trees and Shrubs. New York(New York): Houghton Mifflin;1986:130
- United States Department of Agriculture site.Virginia creeper. 15 Oct 2016. United States Department of Agriculture Natural Resources Conservation Service. https://plants.usda.gov/plantguide/pdf/pg_paqu2.pdf.
Accessed September 4, 2020. - American Academy of Dermatology site. Poison ivy, oak, and sumac: how to treat the rash. https://www.aad.org/public/everyday-care/itchy-skin/poison-ivy/treat-rash. Accessed 22 Sep 2020.
- Boyd JE, Rucker J. No ill nature: the surprising history and science of poison ivy and its relatives. 2 Jun 2013. Science History Institute site. https://www.sciencehistory.org/distillations/no-ill-nature-the-surprising-history-and-science-of-poison-ivy-and-its-relatives. Accessed 21 Sep 2020.
- Hauser SC. Nature’s Revenge. New York, New York: Lyons & Burford Publishing Co.; 1996.
- Templeton D. Climate change is making poison ivy bigger and badder. 22 Jul 2013. Pittsburg Post Gazette. https://www.post-gazette.com/news/health/2013/07/22/Climate-change-is-making-poison-ivy-grow-bigger-and-badder/stories/201307220149. Accessed 22 Sep 2020.
- Internet Dermatology Society, Inc. site. Botanical dermatology: allergic contact dermatitis from Anacardiaceae and related families. 22 Sept 2014. http://www.
- Pray WS. Poison ivy: The classic contact dermatitis.US Pharm. 2007;32(3):11-15,
Accessed 4 Sept 2020.telemedicine.org/botanica/bot6.htm. - Gladman AC. Toxicodendron dermatitis: poison ivy, oak, and sumac. Wilderness Environ Med. 2006;17(2):120–128. Accessed September 4, 2020.
- Wilson S. How poison ivy works. Flowering plants, shrubs, and trees. 23 Sept 2005. How Stuff Works site. https://science.howstuffworks.com/life/botany/poison-ivy.htm. Accessed September 4, 2020.
- Curtisa G, Lewis AC. Treatment of severe poison ivy: a randomized, controlled trial of long- versus short-course oral prednisone. J Clin Med Res. 2014; 6(6):429–434.
- Chaker AM, Athavaley A. Least-welcome sign of summer. Last updated 22 Jun 2010. The Wall Street Journal site. https://www.wsj.com/articles/SB10001424052748704895204575320883257186258. Accessed 22 Sep 2020.
- Associated Press. Even calamine is on FDA’s list of useless medicines. 27 Aug 1992. Los Angeles Times site. https://www.latimes.com/archives/la-xpm-1992-08-27-mn-6909-story.html. Accessed 22 Sep 2020.

