 J Clin Aesthet Dermatol. 2023;16(6):26–29.
J Clin Aesthet Dermatol. 2023;16(6):26–29.
by Christine Guarnieri Munia, MD; Marcus Morais, MD; Maurício Sato, MD; Meire Parada, MD; and Luiz Eduardo Avelar, MD
Dr. Guarnieri is with a Dermatology Private Practice in São Paulo, Brazil. Dr. Morais is with a Private Office in Belo Horizonte, Brazil. Dr. Sato is with Sociedade Brasileira de Dermatologia in Rio de Janeiro, Brazil. Dr. Avelar is with a Private Office in Belo Horizonte, Brazil. Dr. Parada is with a Private Practice in São Paulo, Brazil.
FUNDING: No funding was provided for this article.
DISCLOSURES: Drs. Morais, Sato, and Avelar are speakers, advisors and investigators of Galderma. Drs. Parada and Guarnieri are speakers for Galderma.
The cumulative process of degeneration induced by years of exposure to extrinsic factors, such as ultraviolet irradiation, personalized diet, and pollution can accelerate the aging process. In fact, photoaging (the characteristic changes to skin induced by chronic UV exposure) is believed to be responsible for almost 80 percent of the skin changes commonly attributed to the aging process.1
During aging, the skin may be affected both in terms of quantity (skin sagging) and quality (changes in skin hydration, appearance of spots, wrinkles, and loss of skin elasticity),2 secondary to a combination of repeated muscle contractions, decrease in skin collagen and elastic fibers content, as well as depletion of hyaluronic acid (HA) and impairment of repair process of connective tissue.3 Collagen content of the skin is reduced as a result of its decreased synthesis and also of dermal fibroblasts number, as well as an excessive breakdown by matrix metalloproteinases.4 The HA concentration declines with age and results in a reduced skin elasticity and water-holding capacity of the skin. The volume of the dermis is decreased, and the tendency to wrinkle is increased.3
Different approaches to improve skin physiology toward that associated with a younger individual have been described in the literature, among which poly-L-Lactic acid (PLLA), and subdermal NASHA small particles injections both have been reported to improve the collagen5 and HA content of facial3 and off-face skin. Both procedures are non-surgical, minimally invasive, and well tolerated. PLLA (Sculptra®) and Restylane® Skinboosters™ (RSB) can be used in combination in different therapy sessions or in the same session, but in distinct areas.6 This paper presents the authors’ recommendations for optimized usage of these products to improve facial skin quality, based on their daily clinical practice.
Poly-L-Lactic acid
PLLA (Sculptra®) is a synthetic, biocompatible, and biodegradable collagen biostimulator, which induces a subclinical controlled inflammatory tissue response after injection. The collagen production occurs in response to the PLLA providing long-term natural correction of soft tissue defects, with a gradual increase in the volume of depressed areas over the first few months.6 In a randomized, controlled, double-blind, multicenter study, PLLA-treated subjects presented a statistically significant increase of skin elasticity, hydration, radiance, and smoothness, corroborating patient and physician perception of skin improvement after PLLA treatment.7
Skinboosters injections
Due to the hygroscopic nature of HA, water is drawn into the dermal extracellular matrix to hydrate and improve skin surface roughness and fine wrinkles.3 Clinical evidence of improved skin quality in facial and off-face skin has been highlighted (Restylane® Skinboosters™ (RSB)); 20mg/mL gel, 3 sessions, 1mL/session, each session 4 weeks apart), with significantly improved skin firmness and viscoelastic properties,8 moisture,9 elasticity,3,10 and significantly decreased skin roughness.9–11 In addition, significant overall improvement in skin elasticity and hydration in the periorbital and perioral lines (12mg/mL gel, 3-session regimen, each session 4 to 6 weeks apart),12 neck and décolleté, (12mg/mL gel)5,13 hands,9,11 and arms (20mg/mL gel, 3 sessions, 1mL/session, each session 4 weeks apart) have been reported. The long-term efficacy has been demonstrated at Weeks 12 and 24 after treatment. The progressive improvement of skin structure over the first six months may be maintained for 9 to 12 months after 2 to 3 sessions.5,9
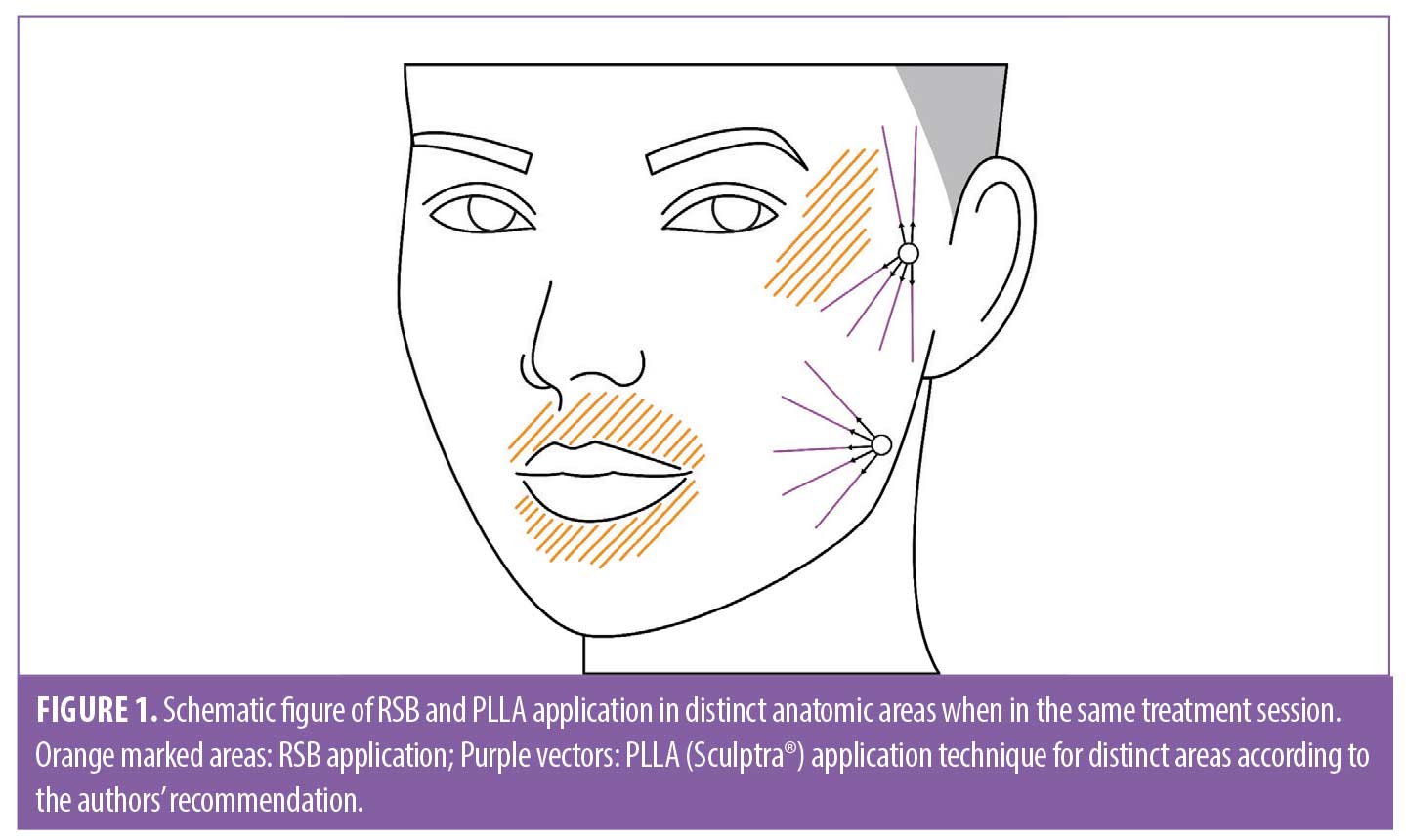
Skin quality improvement in patients with no or mild skin flaccidity
For a patient seeking to improve the skin quality of periorbital and perioral wrinkles and accordion facial lines, injection with RSB would suffice for extracellular matrix remodeling and collagen stimulation. First, the authors recommend a treatment plan that includes 2–3mL RSB facial treatment followed by another injection 30 to 60 days later with 1mL volume (Figure 1- orange marked areas) (Table 1). Once the desired clinical effect is reached, maintenance treatment is suggested every 9 to 12 months.5 Depending on the baseline quality of the skin and the degree of clinical response elicited, the treatment protocol may vary. The youthful face represents a time frame when the bone and soft tissues provide the ideal volume for the overlying skin envelope, leading to smoother skin14 without the need for deep injections for skeletal support. Nevertheless, the use of PLLA (Sculptra®) as a preventative second step measure for the first signs of aging and skin flaccidity, using one vial of PLLA per treatment session (5mL per facial side), is recommended in aiming for collagen stimulation of the facial frame. PLLA (Sculptra®) injections should be performed up to 90 days after the end of the RSB treatment schedule, especially in the pre-auricular and mandibular aspects of the face (Figure 1) (Table 2). A PLLA treatment approach after the initial RSB sessions are also recommended for younger patients with premature and unexpected facial volume loss (e.g. due to illness, steroid abuse, diet, or genetics), adapted to each patient’s clinical presentation. As maintenance treatment of PLLA the authors recommend this once a year.
Skin Quality improvement in patients with pronounced skin flaccidity
Facial bones are the major cornerstones for defining the overall three-dimensional facial contour because they provide the framework which the soft-tissue envelope rests.15 As aging progresses and bone resorbs, the overlying soft tissues lose support, causing a “folding in” of these tissues known as the concertina effect.14 The zygomatic bone suffers resorption, leading to a “lessening” of the zygomatic prominence, loss of support for the soft tissues, and descent of the mid-face.15 Resorption of the pyriform aperture leads to a collapse of the nasal structure with fall of the nose tip.
For patients with skin flaccidity who also present loss of bone support, especially around the pyriform aperture, the inferior portion of the zygoma and/or the mandible angle, as well as loss of contour of the lower face, authors’ recommend to begin with one session with two vials of PLLA (10 mL per facial side) in an attempt to maintain the integrity of the soft tissue support for a longer period and improve skin flaccidity. Additionally, 1 to 2 sessions may be performed 4 to 6 weeks apart between each session according to the patient needs. (Table 2).
The pre-auricular area is particularly prone to volume loss, since only the superficial fat compartments contribute to the subcutaneous volume. Subcutaneous PLLA injections induce neocollagenesis in the malar area, zygomatic arch, pre-auricular, and mandibular angle providing support to the superficial musculoaponeurotic system (SMAS), slightly pulling up the skin, thereby delaying the normal course of sagging of the face.16 The authors recommend one session a year as a maintenance treatment.
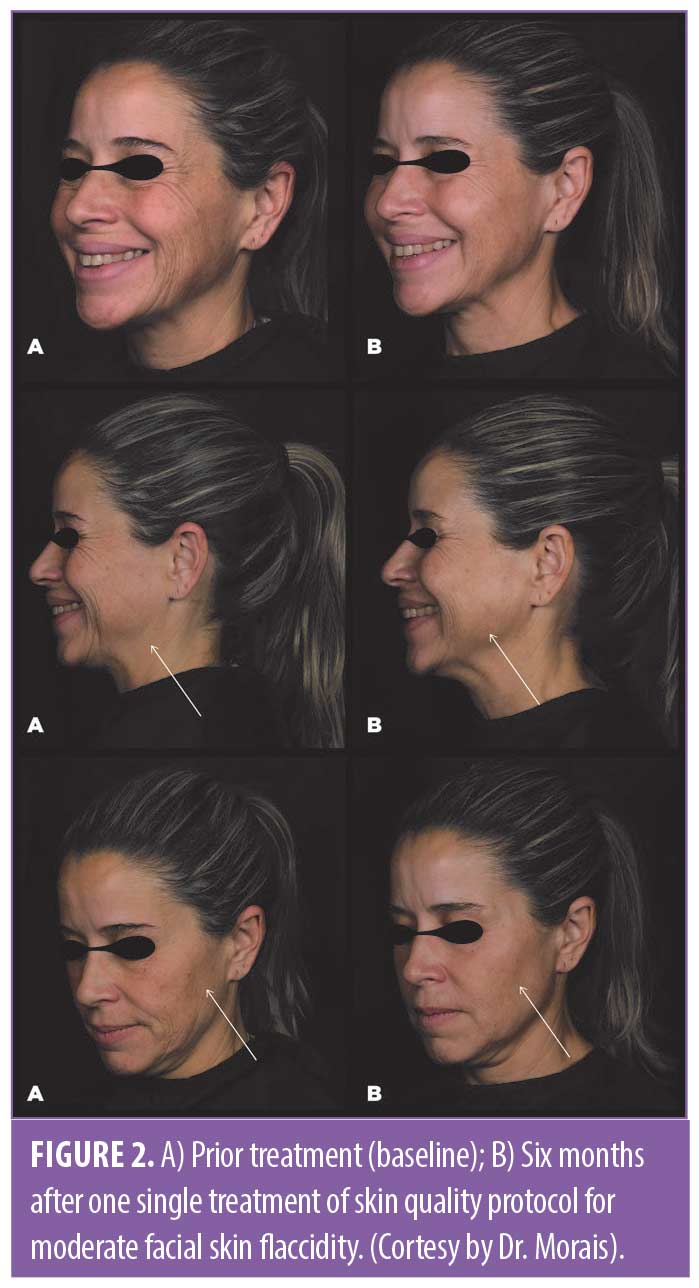
If fine wrinkles and small imperfections remain, the authors suggest 2–3mL RSB application per session for 30 to 60 days, or even three months, after the session of PLLA depending on the clinical assessment in order to complement treatment and achieve the desired outcomes, which could not be achieved solely by PLLA monotherapy. For maintenance treatment, it is worthy to note that each patient may need an additional RSB session after 9 to 12 months from the first session. Figure 2 shows the clinical improvement after six months of one session of the skin quality protocol.
According to the facial assessment and patient profile, PLLA and RSB injections can also be performed in the same session, but in distinct areas: RSB in highly mobile areas with thin subcutaneous tissue in which PLLA is not indicated (e.g., perioral and periorbital zones) and PLLA is injected in the facial frame (Figure 1).
Discussion
The skin is a major indicator of a person’s age, health, and vitality.17 Moreover, skin features (clarity, texture and color) have been reported to be among the key facial features that influence our perception of facial beauty.18
The bony components of the face are important for the overall three-dimensional facial contour because they provide the framework upon which the soft-tissue envelope rests. In the youthful face, the bone and soft tissues occupy the ideal volume for the overlying skin envelope, leading to smoother skin. In contrast, the balance between facial envelope and bony support tends to shift towards excess skin sagging.14 The number and diameter of collagen fiber bundles decrease with age, while the ratio of Type III collagen to Type I collagen increases.19 Degeneration and decreased synthesis of collagen further contribute to the development of an excess skin envelope, wrinkles, and loss of skin elasticity. The decline of the dermal collagen relates to more skin deformation under the same stress conditions, whereas less elastic fibers result in reduced capacity to restore the shape of the skin after the stress is gone. The HA concentration decreases with age, resulting in a reduced elasticity and water-holding capacity in the skin. The volume of the dermis decreases, while the tendency to wrinkle increases.3 Therefore, inducing the formation of new collagen, as well as supplementing HA in order to improve skin physiology toward that associated with a younger individual, is a logical approach. While subdermal RSB injections aim to improve skin hydration, texture, overall skin quality, and collagen synthesis, PLLA injections aim to address the decrease in soft tissue volume and bone loss that occur with aging, as well as induce collagen synthesis and improve skin surface and radiance.
In summary, the authors recommend the use of both PLLA and RSB, becasue of their ability to be minimally invasive, well tolerated, used in the same session, and can be used in the same session, but in distinct facial areas, or if used for the same area, the adequate time between each treatment session should be respected.
The main parameter to choose between either PLLA and/or RSB are the level of skin flaccidity and the overall desired treatment objective.
Acknowledgments
The authors thank Dr. Danielle Shitara and Dr. Cristhine Kamamoto for editorial assistance.
References
- Bonté F, Girard D, Archambault J, et al. Skin Changes During Ageing. In: Harris J. KV, editor. Biochemistry and Cell Biology of Ageing: Part II Clinical Science Subcellular Biochemistry. 91. Singapore: Springer; 2019.
- Sykes JM, Nolen D. Considerations in non-Caucasian facial rejuvenation. Facial Plast Surg Clin North Am. 2014;22(3):463–470.
- Lee BM, Han DG, Choi WS. Rejuvenating Effects of Facial Hydrofilling using Restylane Vital. Arch Plast Surg. 2015;42(3):282–287.
- Helfrich YR, Sachs DL, Voorhees JJ. Overview of skin aging and photoaging. Dermatol Nurs. 2008;20(3):177–183; quiz 84.
- Belmontesi M, De Angelis F, Di Gregorio C, et al. Injectable Non-Animal Stabilized Hyaluronic Acid as a Skin Quality Booster: An Expert Panel Consensus. J Drugs Dermatol. 2018;17(1):83–88.
- Alessio R, Rzany B, Eve L, et al. European expert recommendations on the use of injectable poly-L-lactic acid for facial rejuvenation. J Drugs Dermatol. 2014;13(9):1057–1066.
- Bohnert K, Dorizas A, Lorenc P, et al. Randomized, Controlled, Multicentered, Double-Blind Investigation of Injectable Poly-L-Lactic Acid for Improving Skin Quality. Dermatol Surg. 2019;45(5):718–724.
- Reuther T, Bayrhammer J, Kerscher M. Effects of a three-session skin rejuvenation treatment using stabilized hyaluronic acid-based gel of non-animal origin on skin elasticity: a pilot study. Arch Dermatol Res. 2010;302(1):37–45.
- Gubanova EI, Starovatova PA, Rodina MY. 12-month effects of stabilized hyaluronic acid gel compared with saline for rejuvenation of aging hands. J Drugs Dermatol. 2015;14(3):288–298.
- Kerscher M, Bayrhammer J, Reuther T. Rejuvenating influence of a stabilized hyaluronic acid-based gel of nonanimal origin on facial skin aging. Dermatol Surg. 2008;34(5):720–726.
- Williams S, Tamburic S, Stensvik H, et al. Changes in skin physiology and clinical appearance after microdroplet placement of hyaluronic acid in aging hands. J Cosmet Dermatol. 2009;8(3):216–225.
- Gubanova YI, Diyachenko YY, Rodina MY, et al. Brand-new Hydrobalance technology on the basis of stabilized hyaluronic acid for long-term skin hydration. Vestnik dermatologii i venerologii. 2010;86:94–98.
- Streker M, Reuther T, Krueger N, et al. Stabilized hyaluronic acid-based gel of non-animal origin for skin rejuvenation: face, hand, and decolletage. J Drugs Dermatol. 2013;12(9):990–994.
- Aguilera SB, Branch S, Soro L. Optimizing Injections of Poly-L-lactic Acid: The 6-Step Technique. J Drugs Dermatol. 2016;15(12):1550–1556.
- Avelar LET, Cazerta CEP, Ave MN, et al. Dynamic Changes of Facial Supporting Cornerstones (Pillars): Considerations in Aesthetic Approach. J Drugs Dermatol. 2018;17(4):466–470.
- Hexsel D, Hexsel CL, Cotofana S. Introducing the L-Lift-A Novel Approach to Treat Age-Related Facial Skin Ptosis Using A Collagen Stimulator. Dermatol Surg. 2019.
- Vleggaar D. Facial volumetric correction with injectable poly-L-lactic acid. Dermatol Surg. 2005;31(11 Pt 2):1511–1527; discussion 7–8.
- Swift A, Remington K. BeautiPHIcation: A global approach to facial beauty. Clin Plast Surg. 2011;38(3):347–377.
- Khavkin J, Ellis DA. Aging skin: histology, physiology, and pathology. Facial Plast Surg Clin North Am. 2011;19(2):229–234.

