 J Clin Aesthet Dermatol. 2022;15(6):68-75.
J Clin Aesthet Dermatol. 2022;15(6):68-75.
by Akshitha Thatiparthi, BS; Amylee Martin, BS; Jeffrey Liu, BS; and Jashin J. Wu, MD
Ms. Thatiparthi is with Western University of Health Sciences in Pomona, California. Ms. Martin is with the School of Medicine at University of California in Riverside, California. Mr. Liu is with the Keck School of Medicine at the University of Southern California in Los Angeles, California. Dr. Wu is with the Dermatology Research and Education Foundation in Irvine, California.
FUNDING: No funding was provided for this study.
DISCLOSURES: The author reports no conflicts of interest relevant to the content of this article.
ABSTRACT: Phototherapy is a standard treatment for moderate-to-severe psoriasis. However, concern remains regarding the associated cutaneous carcinogenic risk. Our objective is to conduct a systematic review of skin cancer risk for psoriasis patients treated with phototherapy. To achieve our goal, we searched Cochrane, PubMed, and Embase databases. We aimed to evaluate existing literature (from July 1, 2010, to December 31, 2020) on phototherapy for all Fitzpatrick skin phototypes (FSP) which includes 71 articles, and eight articles being categorized in this review. Five studies did not report an increased skin cancer risk with narrowband-ultraviolet blue (UVB) and unspecified UVB for FSP II through VI, with one study not reporting FSP. Three studies did report an increased risk of skin cancer with narrowband-UVB and broadband-UVB for FSP I-VI, with one study also not specifying skin phototypes or UVB phototherapy type. Additionally, a study with psoralen and ultraviolet A with and without narrowband-UVB demonstrated an increased risk of skin cancer in phototypes III and IV. The most commonly reported secondary outcomes with phototherapy were actinic keratosis (123) and solar lentigines (10). Numerous patients were also on additional therapies including methotrexate, acitretin, and biologics. Study limitations include publication bias due to limited number of studies published on this topic in the last ten years along with heterogeneity in reporting. The relationship between phototherapy, psoriasis, and cutaneous oncogenic risk remains contradictory. While phototherapy for psoriasis is an efficacious therapy, further studies are needed to understand the cutaneous oncogenic risk based on FSP to help clinicals tailor treatment recommendations based on skin phototypes.
Keywords: Cancer, phototherapy, psoriasis, PUVA, UVB, melanoma, narrowband UVB, broadband UVB
Since phototherapy was discovered to be an effective psoriasis treatment in the twentieth century, it has been a mainstay therapeutic option for moderate-to-severe psoriasis. 1,2 Skin conditions commonly treated with phototherapy include psoriasis, atopic dermatitis, vitiligo, mycosis fungoides, and morphea.3 The broad therapeutic options for phototherapy can be attributed to its mechanism of action. As ultraviolet light enters the dermis and epidermis, DNA damage and photoproducts are produced. The byproducts and resulting damage induce apoptosis in keratinocytes, fibroblasts, inflammatory cells, and endothelial cells allowing suppression of the inflammatory cascade.3 Further, the local immunosuppression inhibits DNA cell turnover and induces apoptosis of T lymphocytes. As psoriasis results from dysregulation of T cells and dendritic cells causing an inflammatory cascade leading to keratinocyte hyperproliferation, phototherapy is able to induce remission and improve clinical outcomes.4 Two main types of phototherapy are used in the treatment of psoriasis, ultraviolet A (UVA) and ultraviolet B (UVB).
Ultraviolet A phototherapy emits wavelength between 320 and 400 nanometers (nm).3,5 Psoralen is an organic compound, which can be derived from plants or synthetically created. When psoralen is combined with UVA, they generate a greater phototoxic effect. This combination of UVA and psoralen is known as PUVA.3,6 PUVA is able to penetrate deep into the dermis.3 However, utilization of PUVA has declined over the years due to a dose-dependent risk of carcinogenesis and additional adverse effects.7-12
Initial treatments for psoriasis involving UVB included combining the treatment with tar and anthralin paste or oral/topical psoralen in conjunction with UVA irradiation.2 Broadband UVB (BB-UVB), which emits wavelengths between 290 to 320 nm, became an increasingly popular option.2,3 In the 1980s, researchers discovered wavelengths of 311 to 313 nm had superior efficacy compared to BB-UVB.2 Narrowband UVB (NB-UVB) was able to induce greater clinical and histopathological clearance with greater remission rate compared to BB-UVB.13-15 Due to superiority of NB-UVB, the phototherapy type became a standard of care.5
The prescribed dosage of UVB administered depends on either Fitzpatrick skin phototype (FSP) or minimal erythema dose (MED) testing16-18 Fitzpatrick skin phototype is more commonly utilized to determine initial dose and subsequent increase than MED.18 Fitzpatrick skin phototype is a skin classification system used to rank skin phototypes (from I to VI) based on human skin pigmentation and reaction to UV light.16, 19 This ranking system is relevant to our review as a relationship has been established in literature reporting higher FSP are able to better tolerate higher doses of ultraviolet radiation (UVR) compared to lower skin phototypes. Further, erythema resulting from UVR has been correlated with increased cancer risk due to greater DNA damage in lower FSP compared to higher skin phototypes.17, 18, 20-22
As UV light has phototoxic and cariogenic properties, the carcinogenic risk of this treatment modality in psoriasis needs to be evaluated. Recent comprehensive reviews were published in 2010 and 2015 summarizing literature up to 2015 on skin cancer risk with phototherapy.5, 23 However, both studies broadly examined carcinogenic risk of phototherapy in psoriasis patients on Caucasians vs non-Caucasians. Our review’s objective is to conduct a comprehensive review of multiple databases with further examination of cutaneous carcinogenic risk by FSP. Additionally, we hope to categorize recent additional research published on this topic. Overall, we aim to systematically categorize literature on skin cancer risk with PUVA, UVB, NBUVB, and BBUVB, based on skin phototypes, where available. We hope our comprehensive review will help guide physicians in selecting an appropriate therapeutic regime for patients with psoriasis based on specific skin phototypes.
Methods
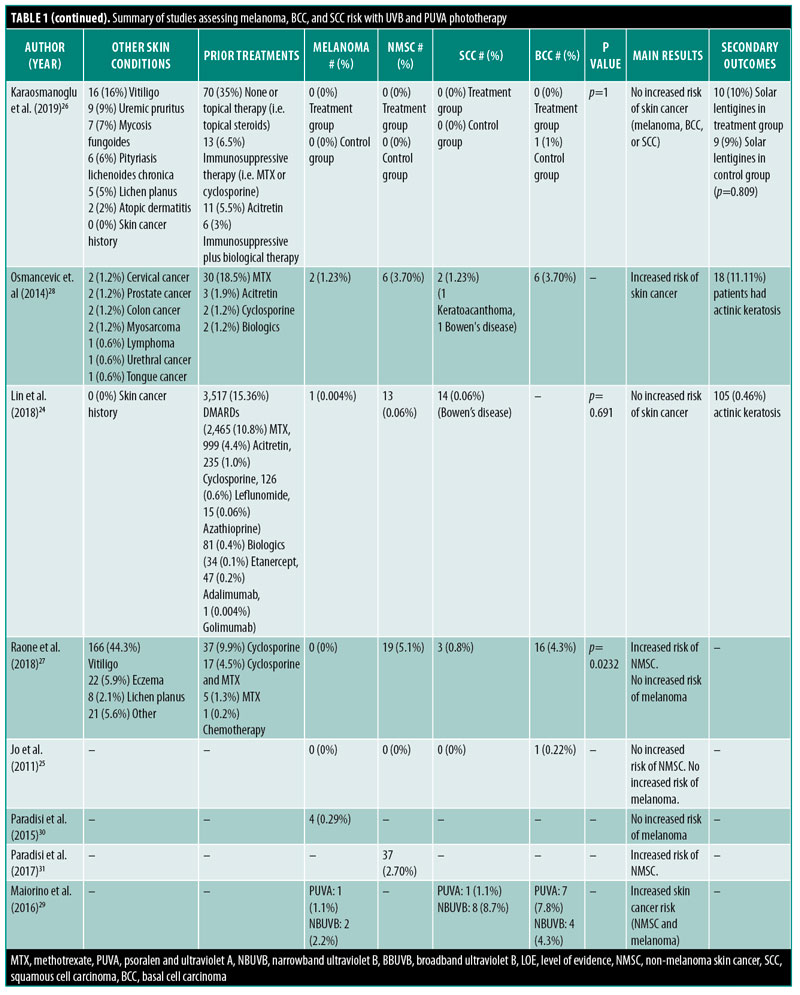
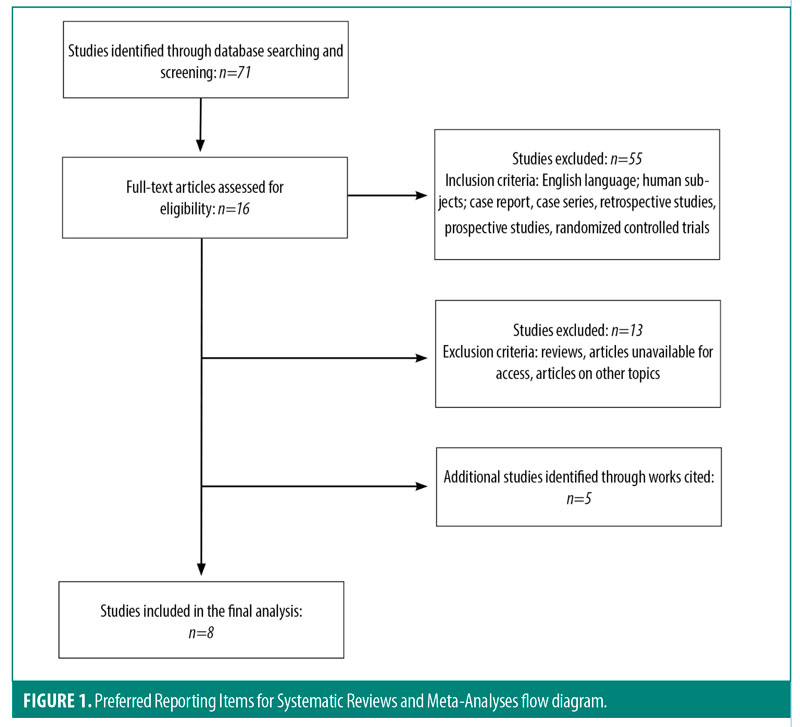
Our systematic review was conducted according to the Preferred Reporting items for Systematic Reviews and Meta-Analyses. Pubmed, Embase and Cochrane databases were queried on December 21, 2020 using the following search terms: “Psoriasis” AND “UVB therapy” AND “skin” AND “cancer” OR “neoplasm” OR “melanoma”. We also utilized the following search terms: “Psoriasis” AND “UVA therapy” AND “skin” AND “cancer” OR “neoplasm” OR “melanoma”. Articles written in English published in the last 10 years were included. Systemic reviews with or without meta-analyses, narrative reviews, and articles with irretrievable records were excluded. After reviewing abstracts and full-text review, only articles pertaining to phototherapy in cancer, and psoriasis were extracted and analyzed. Relevant studies identified through the references of articles during full-text review were added if missed during database searching (Figure 1). Study design, treatment types, patient skin cancer outcomes, and overall results were summarized from each article (Table 1).

Results
Study selection. A total of 71 results were identified from all three databases from July 1, 2010 to December 31, 2020. After removal of duplicates, the search yielded 21 results. Initial screening of text was performed by reviewing article titles and abstracts. Sixteen articles were included for full-text review; thirteen articles were excluded after full-text review. During examination of the bibliography sections, nine additional records were added. A total of eight studies were categorized in this review. These included two cross-sectional studies and six retrospective studies. The selection process of the articles and ranking of the studies by the Oxford Centre for Evidence based medicine are summarized in Figure 1 and Table 1.
Skin cancer risk in specified skin type with NB-UVB. A national cohort study of 22,891 Taiwanese patients with psoriasis with skin phototypes III and IV treated with NB-UVB found one case of melanoma, 13 cases of non-melanoma skin cancer (NMSC), and 14 cases of Bowen’s disease.24 Between the two cohorts, the study did not report a difference in the risk (p=0.691) of skin cancer between long term (≥ 90) and short-term (<90) phototherapy.24 Jo et al25 performed a retrospective cohort study of 445 (358 psoriasis) patients treated with NB-UVB for skin types III-IV (52 skin type III, 92 skin type IV, 40 skin type V, 261 unknown skin type). The study noted no increased risk of NMSC compared to a national skin registry (standardized incidence ratio 17; 95% confidence interval (CI) 0.4-94.8). Also, zero cases of melanoma were reported. The study noted they did not find an increased risk of skin cancer but stated over 25,000 patients need to be examined to achieve statistical significance for results reporting.25
A Turkish study evaluated NB-UVB phototherapy of 100 patients to 100 control patients with skin phototypes with five (5%) phototype II, 92 (92%) phototype III, and three (3%) phototype IV.26 The treatment cohort did not develop a significant risk of skin cancer compared to the control group. Further, the study reported a longer follow-up period and greater number of patients are needed to better elucidate the relationship between NB-UVB and skin cancer.26
Similarly, a study in Italy investigated the effects of NB-UVB used to treat various dermatologic conditions, including vitiligo and psoriasis.27 The skin types of patients include 131 (34.9%) skin phototype II, 202 (53.9%) skin phototype III, 30 (8.0%) skin phototype IV, and 12 (3.2%) skin phototypes I, V, VI.[27] Overall, the study reported an increased risk of NMSC (p=0.02), without an increased risk of melanoma. Raone et al27 found patients who received a lower number of treatment sessions developed NMSC (BCC <299 treatments, SCC <99 treatments). The overall risk of NMSC (2.1%) in the study population was increased compared to general European population NMSC prevalence (1.4%).
Skin cancer risk in specified skin type with BB-UVB and/or NB-UVB. A cross-sectional study by Osmancevic et al28 studied 162 Caucasian patients of 9 (5.6%) skin type I, 26 (16.0%) skin type II, 107 (66.0%) skin type III, 13 (8.0%) skin type IV, and 7 (4.3% ) unknown, treated with BB-UVB, NB-UVB, or both. The study reported an increased risk (4.9%, 0.95 CI 2.2-9.5%) of histopathologically verified skin cancer that was dependent on age and treatment number.28
Skin cancer risk in specified skin type with PUVA and/or NB-UVB. In 2016, Maiorino et al29 retrospectively studied outcomes for 92 patients previously treated with PUVA or NB-U VB. Most of the Italian patients were either skin type III or IV.29 For PUVA therapy, patients treated with less than or equal to 250 sessions had one case of melanoma, while patients with greater than 250 sessions had seven cases of BCC and one case of SCC. With NB-UVB, one case of melanoma was reported with less than or equal to 200 sessions and for greater than 200 sessions, one case of melanoma, nine cases of BCC, and eight cases of SCC were found.29 This study advised against high number of phototherapy sessions in darker III and IV skin phototypes as there was a risk of skin cancer with these skin types.29
Skin cancer risk in unspecified skin type and unspecified phototherapy. Paradisi et 30, 31 al. completed two large retrospective cohort studies in Italy. The first study compared 72,739 patients with psoriasis to a referent cohort of 25,956 non-dermatologic vascular surgery patients for risk of melanoma.30 Out of the 1,372 treated with phototherapy for psoriasis, four (2.9%) patients developed melanoma. However, the study reported a non-significant increased risk for melanoma (adjusted odds ratio (aOR) 1.50, 95% CI 0.56-4.15, p=0.402).30 The second study similarly examined 1,372 patients for the risk of NMSC.31 A total of 300 patients were treated with phototherapy, with four patients developing NMSC. Paradisi et al31 reported a significant increased risk of NMSC compared to the control group (aOR 2.67, 95% CI 1.89-3.75, p<0.001). Neither of the studies specified phototherapy type nor skin phototype.30, 31
Prior treatments. Additionally, four of the studies reported concomitant medications (3,974) for patients.24, 26-28 In descending order, the most common medications were: 2,470 methotrexate, 1,013 acitretin, 274 cyclosporine, 83 biologics, 70 none or topical therapies (i.e. topical steroids), 17 cyclosporine and methotrexate, 15 azathioprine, 13 immunosuppressive therapies (i.e. methotrexate, cyclosporine), 12 leflunomide, 6 biologics and immunosuppressive therapies, and 1 chemotherapy.
Comorbid skin conditions and secondary outcomes. Dermatologic conditions other than psoriasis were reported 273 times. Vitiligo (182) was the most common condition and pityriasis lichenoides chronica (6) was least commonly observed skin condition. Twenty-one cases of non-skin cancer were observed in patient histories. Moreover, as a result of the phototherapy, 123 cases of actinic keratosis and 10 cases of solar lentigines were reported.
Discussion
As the cutaneous oncogenic risk based on skin phototype remains poorly reported in literature, our study conducted a systematic review of this topic. We evaluated 71 articles and categorized eight articles published from December 2010 to December 2020. Majority (5/8) of the studies evaluated in our study did not report an increased risk of skin cancer in FSP phototypes II-VI. However, three studies did report an increased risk of skin cancer in skin types I-VI. Additionally, in patients with psoriasis and darker skin phototypes, a dose dependent increased cancer risk with PUVA and/or NB-UVB was noted in one report. Overall, due to contradictory evidence and limited reporting of FSP in studies evaluated, strong conclusions cannot be drawn about the oncogenic risk in psoriasis patients based on skin phototypes. Clinicians should make continue to make recommendations for patients on a case-by-case basis with respect to preference and medical history.
Several previous studies demonstrated an significantly increased risk of SCC with PUVA with a non-significant increased risk for BCC in exposed and un-exposed areas for psoriasis patients.5, 10, 32-38 However, Chen et al7, 39, 40 did not report a significant increase in cancer risk (adjusted hazard ratio (HR) 1.1, 95% CI 0.58-2.28) with PUVA, which is consistent with two additional European studies reporting no increased risk of melanoma with PUVA. As cutaneous oncogenic risk based on skin phototype with PUVA remains contraindicatory, NB-UVB is a good alternative option.23, 41-46 Chen et al39 also noted that UVB reduced the risk (adjusted HR 0.52, 95% CI 0.29-0.95, p=0.03) of cancer in patients with psoriasis compared to control. Similarly, a meta-analysis did not report a significant carcinogenic risk, including melanoma, in patients with psoriasis treated with phototherapy or systemic treatments (HR=1.09, 95% CI 0.74–1.63).47 A population-based epidemiology study by Fuxench et al48 reported risk of NMSC was highest for patients who received phototherapy or systematic treatments for psoriasis. Overall, high exposure to UV light from increased phototherapy treatment sessions may increase cutaneous oncogenic risk for all skin phototypes.29, 49 Caution is advised with greater than 250 sessions of PUVA and 300 sessions of UVB, as UVB and PUVA may have an synergistic effect in increasing skin cancer.8, 25, 29
Skin phototype should be considered when interpreting results regarding phototherapy related cutaneous cancer risk due to variances in reactions to factors, such as UV exposure.50 Numerous studies have been conducted on Caucasian patients for risk of skin cancer with phototherapy.44, 51, 52 Thus, lighter skin phototypes (I/II) are well-studied for these factors.2, 53, 54 However, darker phototypes have increased morbidity and mortality for skin cancer due to atypical lesions or advanced stage at presentation. A potential reason for the worse outcomes in skin of color are increase socioeconomic barriers to accessing care.54, 55 Increased education for patients of all phototypes and screening could help mitigate adverse outcomes.
Numerous patients in the studies included in this review were previously treated with additional medications. Studies have reported an increase in skin cancer with systemic biologics and immunosuppressants.12, 56-58 The medications could be a confounding factor for skin cancer risk with phototherapy. Similarly, patients may have a diagnosis of additional skin conditions or cancers increasing cutaneous oncogenic risk.59, 60 Long term trials and pharmacovigilance studies, with reporting of additional concomitant treatment modalities and comorbid conditions, will provide further insights into the risk of cutaneous malignancy by FSP in psoriasis patients.58
Strengths for studies include extensive review of three databases. Our study also uniquely reported on cutaneous carcinogenic risk based on skin phototype, which has limited reports in literature. Moreover, only a few studies investigating the relationship between phototherapy and cancer risk in psoriasis patients were published in the last ten years. Specifically, studies with PUVA in patients with psoriasis were limited. Owing to the eight limited studies published, the risk of skin cancer in patients with psoriasis may be underreported compared to the general population. Many articles did not specifically report melanoma and NMSC risk by FSP, which limited categorization of study results. Moreover, the extent of phototherapy exposure was seldom reported affecting the strength of conclusions drawn by the studies.
Further long-term studies and clinical trials regarding the phototherapy and patients with psoriasis by phototype are needed to draw stronger conclusions, especially for darker FSP. While phototherapy is an efficacious treatment option with a mild side effect profile, a decreasing trend has been found for the prescription of the treatment modality in psoriasis. Recent advancements have increased availability treatment options including biologics, biosimilars, non-biologic systemic immunosuppressants, with numerous clinical trials supporting the safety and efficacy of additional treatment options might be the cause for the decreasing trend.61 Clinicians should consider phototherapy a viable treatment option for psoriasis even during COVID-19, where home phototherapy is an option for patients who do not have pre-pandemic access to office-based phototherapy practices or infusion treatments.62 Additionally, risks versus benefits of phototherapy should be considered on a case-by-case basis while prescribing the treatment modality.
Conclusion
As a fundamental treatment option for moderate-to-severe psoriasis, phototherapy has demonstrated efficacy, safety, and safety profiles for affected patients. However, concern for cutaneous oncogenic risk remains. The results of this systematic review should be interpreted with caution as current evidence is heterogenous in nature, impeding the ability to draw strong conclusions. Most studies examined in our systematic review did not demonstrate an increased cutaneous oncogenic risk for phototherapy, however data exists supporting skin cancer risk. Future studies on this topic should increase categorization of patients based on FSP in phototherapy for psoriasis, with comparison of skin cancer risk between individuals with lighter and darker phototypes when possible.
References
- Wong T, Hsu L, Liao W. Phototherapy in psoriasis: a review of mechanisms of action. J Cutan Med Surg. 2013 Jan-Feb;17(1):6–12.
- Menter A, Korman NJ, Elmets CA, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: Section 5. Guidelines of care for the treatment of psoriasis with phototherapy and photochemotherapy. Journal of the American Academy of Dermatology. 2010;62(1):114–135.
- Vangipuram R, Feldman S. Ultraviolet phototherapy for cutaneous diseases: a concise review. Oral Diseases. 2016;22(4):253–259.
- Boehncke W-H, Schön MP. Psoriasis. The Lancet. 2015 2015/09/05/;386(9997):983–994.
- Wang E, Sasaki J, Nakamura M, et al. Cutaneous Carcinogenic Risk of Phototherapy: An Updated Comprehensive Review. Journal of Psoriasis and Psoriatic Arthritis. 2015;1(1):44–51.
- Shenoi SD, Prabhu S. Photochemotherapy (PUVA) in psoriasis and vitiligo. Indian J Dermatol Venereol Leprol. 2014 Nov-Dec;80(6):497–504.
- McKenna KE, Patterson CC, Handley J, et al. Cutaneous neoplasia following PUVA therapy for psoriasis. Br J Dermatol. 1996 Apr;134(4):639–642.
- Stern RS, Nichols KT, Väkevä LH. Malignant melanoma in patients treated for psoriasis with methoxsalen (psoralen) and ultraviolet A radiation (PUVA). The PUVA Follow-Up Study. N Engl J Med. 1997 Apr 10;336(15):1041–1045.
- Stern RS. The risk of melanoma in association with long-term exposure to PUVA. J Am Acad Dermatol. 2001 May;44(5):755–761.
- Stern RS. The risk of squamous cell and basal cell cancer associated with psoralen and ultraviolet A therapy: a 30-year prospective study. J Am Acad Dermatol. 2012 Apr;66(4):553–562.
- Lunder EJ, Stern RS. Merkel-cell carcinomas in patients treated with methoxsalen and ultraviolet A radiation. N Engl J Med. 1998 Oct 22;339(17):1247–1248.
- Geller S, Xu H, Lebwohl M, et al. Malignancy Risk and Recurrence with Psoriasis and its Treatments: A Concise Update. American Journal of Clinical Dermatology. 2018;19(3):363–375.
- Karvonen J, Kokkonen EL, Ruotsalainen E. 311 nm UVB lamps in the treatment of psoriasis with the Ingram regimen. Acta Derm Venereol. 1989;69(1):82–85.
- Walters IB, Burack LH, Coven TR, et al. Suberythemogenic narrow-band UVB is markedly more effective than conventional UVB in treatment of psoriasis vulgaris. J Am Acad Dermatol. 1999 Jun;40(6 Pt 1):893–900.
- Coven TR, Burack LH, Gilleaudeau R, et al. Narrowband UV-B produces superior clinical and histopathological resolution of moderate-to-severe psoriasis in patients compared with broadband UV-B. Arch Dermatol. 1997 Dec;133(12):1514–1522.
- Gupta V, Sharma VK. Skin typing: Fitzpatrick grading and others. Clin Dermatol. 2019 Sep-Oct;37(5):430–436.
- Menter A, Gottlieb A, Feldman SR, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: Section 1. Overview of psoriasis and guidelines of care for the treatment of psoriasis with biologics. J Am Acad Dermatol. 2008 May;58(5):826–850.
- Hum M, Kalia S, Gniadecki R. Prescribing Home Narrowband UVB Phototherapy: A Review of Current Approaches. J Cutan Med Surg. 2019 Jan/Feb;23(1):91–96.
- Sharma AN, Patel BC. Laser Fitzpatrick Skin Type Recommendations. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2021, StatPearls Publishing LLC.; 2021.
- Palmer RA, Aquilina S, Milligan PJ, et al. Photoadaptation during Narrowband Ultraviolet-B Therapy Is Independent of Skin Type: A Study of 352 Patients. Journal of Investigative Dermatology. 2006;126(6):1256–1263.
- Young AR. Chromophores in human skin. Physics in Medicine and Biology. 1997;42(5):789–802.
- Young AR, Chadwick CA, Harrison GI, et al. The similarity of action spectra for thymine dimers in human epidermis and erythema suggests that DNA is the chromophore for erythema. J Invest Dermatol. 1998 Dec;111(6):982–988.
- Archier E, Devaux S, Castela E, et al. Carcinogenic risks of psoralen UV-A therapy and narrowband UV-B therapy in chronic plaque psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2012 May;26 Suppl 3:22–31.
- Lin T-L, Wu C-Y, Chang Y-T, et al. Risk of skin cancer in psoriasis patients receiving long-term narrowband ultraviolet phototherapy: Results from a Taiwanese population-based cohort study. Photodermatol Photoimmunol Photomed. 2019 May;35(3):164-171.
- Jo SJ, Kwon HH, Choi MR, et al. No Evidence for Increased Skin Cancer Risk in Koreans with Skin Phototypes III-V Treated with Narrowband UVB Phototherapy. Acta Derm Venereol. 2011 Jan;91(1):40-43.
- Karaosmanoglu N, Ozdemir Cetinkaya P, Kutlu O, Karaaslan E, et al. A cross-sectional analysis of skin cancer risk in patients receiving narrow-band ultraviolet B phototherapy: an evaluation of 100 patients. Archives of Dermatological Research. 2020;312(4):249.
- Raone B, Patrizi A, Gurioli C, et al. Cutaneous carcinogenic risk evaluation in 375 patients treated with narrowband-UVB phototherapy: A 15-year experience from our Institute. Photodermatol Photoimmunol Photomed. 2018 Sep;34(5):302-306.
- Osmancevic A, Gillstedt M, Wennberg A-M, Larko O. The Risk of Skin Cancer in Psoriasis Patients Treated with UVB Therapy. Acta Derm Venereol. 2014 Jul;94(4):425-30.
- Maiorino A, De Simone C, Perino F, et al. Melanoma and non-melanoma skin cancer in psoriatic patients treated with high-dose phototherapy. J Dermatolog Treat. 2016 Oct;27(5):443-7.
- Paradisi A, Tabolli S, Didona B, et al. Reduced frequency of melanoma in 72,739 patients with psoriasis: A retrospective study. European Journal of Dermatology. 2015;25(2):133.
- Paradisi A, Didona B, Tabolli S, et al. Reduced frequency of non-melanoma skin cancer in 72,739 patients with psoriasis: a retrospective study. Eur J Dermatol. 2017 Aug 1;27(4):359-362.
- Stern RS, Laird N, Melski J, et al. Cutaneous squamous-cell carcinoma in patients treated with PUVA. N Engl J Med. 1984 May 3;310(18):1156-1161.
- Stern RS, Lange R. Non-melanoma skin cancer occurring in patients treated with PUVA five to ten years after first treatment. J Invest Dermatol. 1988 Aug;91(2):120–124.
- Stern RS. Genital tumors among men with psoriasis exposed to psoralens and ultraviolet A radiation (PUVA) and ultraviolet B radiation. The Photochemotherapy Follow-up Study. N Engl J Med. 1990 Apr 19;322(16):1093–1097.
- Stern RS, Laird N. The carcinogenic risk of treatments for severe psoriasis. Photochemotherapy Follow-up Study. Cancer. 1994 Jun 1;73(11):2759–2764.
- Stern RS, Liebman EJ, Väkevä L. Oral psoralen and ultraviolet-A light (PUVA) treatment of psoriasis and persistent risk of nonmelanoma skin cancer. PUVA Follow-up Study. J Natl Cancer Inst. 1998 Sep 2;90(17):1278–1284.
- Stern RS, Bagheri S, Nichols K. The persistent risk of genital tumors among men treated with psoralen plus ultraviolet A (PUVA) for psoriasis. J Am Acad Dermatol. 2002 Jul;47(1):33–39.
- Katz KA, Marcil I, Stern RS. Incidence and risk factors associated with a second squamous cell carcinoma or basal cell carcinoma in psoralen + ultraviolet a light-treated psoriasis patients. J Invest Dermatol. 2002 Jun;118(6):1038–1043.
- Chen Y-J, Wu C-Y, Chen T-J, et al. The risk of cancer in patients with psoriasis: A population-based cohort study in Taiwan. Journal of the American Academy of Dermatology. 2011 01/01/January 2011;65(1):84–91.
- Bruynzeel I, Bergman W, Hartevelt HM, et al. ‘High single-dose’ European PUVA regimen also causes an excess of non-melanoma skin cancer. Br J Dermatol. 1991 Jan;124(1):49–55.
- Lindelöf B, Sigurgeirsson B, Tegner E, et al. PUVA and cancer risk: the Swedish follow-up study. Br J Dermatol. 1999 Jul;141(1):108–112.
- Lim JL, Stern RS. High levels of ultraviolet B exposure increase the risk of non-melanoma skin cancer in psoralen and ultraviolet A-treated patients. J Invest Dermatol. 2005 Mar;124(3):505–513.
- Murase JE, Lee EE, Koo J. Effect of ethnicity on the risk of developing nonmelanoma skin cancer following long-term PUVA therapy. Int J Dermatol. 2005 Dec;44(12):1016–1021.
- Hearn RM, Kerr AC, Rahim KF, et al. Incidence of skin cancers in 3867 patients treated with narrow-band ultraviolet B phototherapy. Br J Dermatol. 2008 Sep;159(4):931–935.
- Chen X, Yang M, Cheng Y, et al. Narrow-band ultraviolet B phototherapy versus broad-band ultraviolet B or psoralen-ultraviolet A photochemotherapy for psoriasis. Cochrane Database Syst Rev. 2013 Oct 23(10):Cd009481.
- Beani JC, Jeanmougin M. [Narrow-band UVB therapy in psoriasis vulgaris: good practice guideline and recommendations of the French Society of Photodermatology]. Ann Dermatol Venereol. 2010 Jan;137(1):21–31.
- Pouplard C, Brenaut E, Horreau C, et al. Risk of cancer in psoriasis: a systematic review and meta-analysis of epidemiological studies. J Eur Acad Dermatol Venereol. 2013 Aug;27 Suppl 3:36–46.
- Chiesa Fuxench ZC, Shin DB, Ogdie Beatty A, et al. The Risk of Cancer in Patients With Psoriasis: A Population-Based Cohort Study in the Health Improvement Network. JAMA Dermatol. 2016 Mar;152(3):282–290.
- Kozma B, Eide MJ. Photocarcinogenesis: an epidemiologic perspective on ultraviolet light and skin cancer. Dermatol Clin. 2014 Jul;32(3):301–313, viii.
- Jo SJ, Yoon HS, Woo SM, et al. Time course of tanning induced by narrow-band UVB phototherapy in Korean psoriasis patients. Photodermatol Photoimmunol Photomed. 2006 Aug;22(4):193–199.
- Weischer M, Blum A, Eberhard F, et al. No evidence for increased skin cancer risk in psoriasis patients treated with broadband or narrowband UVB phototherapy: a first retrospective study. Acta Derm Venereol. 2004;84(5):370–374.
- Black RJ, Gavin AT. Photocarcinogenic risk of narrowband ultraviolet B (TL-01) phototherapy: early follow-up data. Br J Dermatol. 2006 Mar;154(3):566–567.
- Ibbotson SH, Bilsland D, Cox NH, et al. An update and guidance on narrowband ultraviolet B phototherapy: a British Photodermatology Group Workshop Report. Br J Dermatol. 2004 Aug;151(2):283–297.
- Bradford PT. Skin cancer in skin of color. Dermatol Nurs. 2009 Jul-Aug;21(4):170–177, 206; quiz 178.
- Gupta AK, Bharadwaj M, Mehrotra R. Skin Cancer Concerns in People of Color: Risk Factors and Prevention. Asian Pac J Cancer Prev. 2016 Dec 1;17(12):5257–5264.
- Patel RV, Clark LN, Lebwohl M, et al. Treatments for psoriasis and the risk of malignancy. J Am Acad Dermatol. 2009 Jun;60(6):1001–1017.
- Naldi L. Malignancy concerns with psoriasis treatments using phototherapy, methotrexate, cyclosporin, and biologics: facts and controversies. Clin Dermatol. 2010 Jan-Feb;28(1):88–92.
- Peleva E, Exton LS, Kelley K, et al. Risk of cancer in patients with psoriasis on biological therapies: a systematic review. Br J Dermatol. 2018 Jan;178(1):103–113.
- Cho HG, Kuo KY, Li S, et al. Frequent basal cell cancer development is a clinical marker for inherited cancer susceptibility. JCI Insight. 2018 Aug 9;3(15).
- Green A, Whiteman D, Frost C, et al. Sun exposure, skin cancers and related skin conditions. J Epidemiol. 1999 Dec;9(6 Suppl):S7–S13.
- Amin M, No DJ, Egeberg A, et al. Choosing First-Line Biologic Treatment for Moderate-to-Severe Psoriasis: What Does the Evidence Say? Am J Clin Dermatol. 2018 Feb;19(1):1–13.
- Thatiparthi A, Martin A, Liu J, Wu J. Home Phototherapy During the COVID-19 Pandemic. Cutis. 2021 Feb;107(2):87-88.

