 J Clin Aesthet Dermatol. 2021;14(7):26–28.
J Clin Aesthet Dermatol. 2021;14(7):26–28.
by Christine Braegelmann, MD; Dennis Niebel, MD; Joerg Wenzel, MD; and Thomas Bieber, MD
All authors are with the Department of Dermatology and Allergy at the University Hospital Bonn in Bonn, Germany.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Neutrophilic dermatosis of the dorsal hands (NDDH) is considered a localized variant of acute febrile neutrophilic dermatosis. It is a rare condition and presents with erythematous tender nodules and plaques on the extensor sides of the hands. Forty percent of NDDH cases occur in association with an underlying disease, with hematologic disorders being the most frequent type. Here, we describe the case of a 77-year-old male patient who presented with acute tumid, erythematous lesions of the fingers. As part of this report, we discuss possible differential diagnoses of NDDH and seek to raise awareness of this rare condition, as misdiagnoses often lead to a delay in adequate treatment and thus more dramatic disease courses.
Keywords: Neutrophilic dermatosis of the dorsal hands, neutrophilic fixed drug eruption, erysipela, erythema elevatum et diutinum, glucocorticoid treatment
Neutrophilic dermatosis of the dorsal hands (NDDH) presents as a localized variant of acute febrile neutrophilic dermatosis (i.e., Sweet syndrome) and was first described by Galaria et al1 in 2000. Before this, a clinically similar phenomenon was characterized as “pustular vasculitis of the hands” in patients showing histological features of leukocytoclastic vasculitis.2 It is likely that the vasculitis is secondary due to the intensity of the neutrophilic infiltration, and thus, is dependent on the timing of biopsy during evolution of the lesion.3
Case Presentation
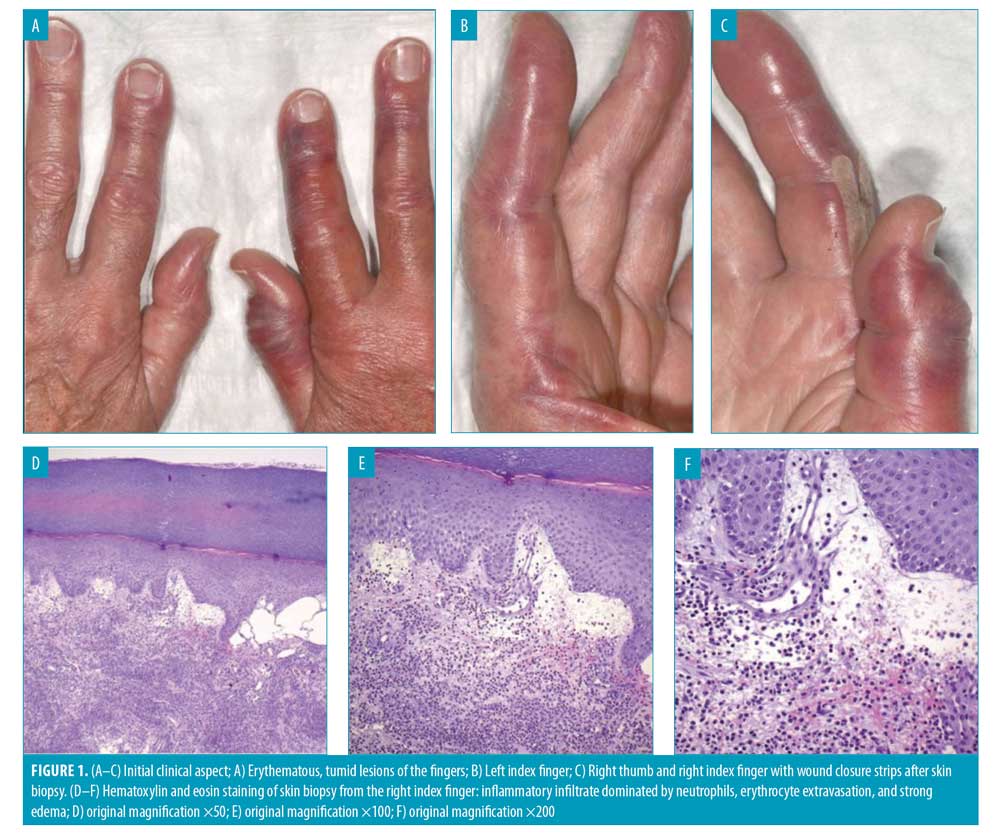
A 77-year-old male patient presented with tumid, erythematous lesions of the fingers that showed grayish, pseudo-bullous aspects in their central areas (Figures 1A–C). The findings correlated with moderate local warmth. Seven days prior to consultation, proton-pump inhibitor therapy was initiated due to heartburn. After five days, the patient stopped this therapy upon first recognition of a small erythematous lesion on the dorsal side of the right index finger. However, the lesions progressed in spite of drug discontinuation. Apart from moderate burning pain at the site of the lesion, the patient felt well and had no fever or chills. His general practitioner administered an infusion of glucocorticoids before referring him to our department directly afterwards. The patient reported a slight alleviation of persistent pain after the infusion. He reported a weight loss of seven percent over the previous six months and occasional pipe smoking. Laboratory investigations showed an elevated C-reactive protein level of 52.48mg/L (normal range: 0–3mg/L) and leukocytosis with a leukocyte concentration of 12.84G/L (normal range: 3.8-10.5G/L), with pronounced neutrophilia. Histological analysis of a lesional skin biopsy of the right index finger revealed a marked inflammatory infiltrate dominated by neutrophils permeating the connective tissue and also affecting vascular structures, erythrocyte extravasation and strong edema (Figures 1D–F). After discussing possible differential diagnoses outlined later in this paper, we considered NDDH to be the most likely diagnosis. Upon further examination of our patient, we detected Bence-Jones protein in the urine. Computed tomography, however, showed no evidence of myeloma. Dual corticosteroid therapy (1mg/kg of body weight of prednisolone, once daily orally, and mometasonfuroat cream, once daily topically) was initiated. At his request, the patient was released from the hospital three days after initial consultation free of pain, in incipient remission regarding edema and erythema, and with improved laboratory values (C-reactive protein level of 12.2mg/L, leukocyte concentration of 11.49G/L, and no detectable neutrophilia). During a follow-up visit four days later, the lesions were almost completely resolved, showing exfoliation of the affected skin areas in large scale-like flakes, which hold evidence of the preceding tissue damage (Figure 2). Glucocorticoid tapering was carried out continuously over a period of three months. Six months after first consultation, the patient had not experienced any relapse. He regularly visits his general practitioner for follow up regarding the detected Bence-Jones protein.

Discussion
As a possible differential diagnosis, we considered fixed drug eruption (FDE), which usually features well-demarcated dusky red macules or edematous plaques with optional blistering. Upon repeated drug ingestion, it recurs in the same location, most likely due to effector-memory T-cell populations residing in the epithelial tissue.4 Histologically, FDE features a lichenoid tissue reaction characterized by lymphocytic infiltration with hydropic degeneration of basal keratinocytes.5 Several reports, however, have introduced the phenomenon of neutrophilic FDE (nFDE), which clinically meets the criteria of FDE but shows predominant neutrophilic infiltration in histological specimens.6 However, neutrophilic infiltration to the extent observed in our patient’s skin is not described. Classical findings of FDE, such as scattered necrotic keratinocytes, are also described in the case of nFDE and were absent in our patient’s biopsy. Erysipelas must also be recognized as a possible differential diagnosis, as its clinical picture is characterized by local signs of inflammation, such as erythema, warmth, and pain.7 Manifestation on the arm/hand is the second most common site of infection after the leg.8 Bilateral manifestation and lack of commonly associated symptoms, such as fever and nausea,9 however, aided in the dismissal of erysipelas as a probable differential diagnosis. A further possible differential diagnosis is erythema elevatum et diutinum (EED), which features yellowish to red-brown plaques, papules, or nodules,10 whereas NDDH typically shows erythematous plaques.11 Both diseases predominantly affect the extensor surfaces of the hands and most often occur bilaterally.10,11 The acute manifestation within only a few days, however, was evidence against EED, because one of its key features is a persistent, chronic course of disease.10 Furthermore, peripheral neutrophilia is not a typical feature of EED as described in the literature and, as opposed to NDDH, the histopathology of EED is characterized by cutaneous leukocytoclastic vasculitis also in early stages.12
In consideration of the criteria discussed, NDDH seemed to be the most likely differential diagnosis. Concerning our patient, a drug-induced manifestation seems possible, as proton-pump inhibitors are suggested to be possible triggers of neutrophilic dermatosis.13 The excellent therapeutic effect upon glucocorticoid administration further supported this diagnosis, as rapid response to glucocorticoids is a hallmark of NDDH.11
About 40 percent of NDDH cases occur in association with an underlying disease; the most frequently detected pathologies are hematologic disorders (e.g., gammopathies, myelodysplasias or malignancies), recent infections, solid organ tumors, and inflammatory bowel diseases.11 This association makes further examination of NDDH patients inevitable.
Conclusion
The given case report highlights the initial stage of NDDH and a favorable course of disease. A review of the literature, however, revealed that, because of its clinical appearance, NDDH tends to be misdiagnosed, leading to a delay in adequate treatment and thus dramatic courses of disease.14 With this case, we aim to raise awareness of the rare condition of NDDH, which must be considered in patients with tender erythematous lesions on the dorsal hands. An early, correct diagnosis allows for necessary further examination in patients with NDDH, and subsequent sufficient therapeutic management leads to regression before the condition progresses to an ulcerating stage of disease, as described elsewhere.14,15
References
- Galaria NA, Junkins-Hopkins JM, Kligman D, James WD. Neutrophilic dermatosis of the dorsal hands: pustular vasculitis revisited. J Am Acad Dermatol. 2000;43(5 Pt 1):870–874.
- Strutton G, Weedon D, Robertson I. Pustular vasculitis of the hands. J Am Acad Dermatol. 1995;32(2 Pt 1):192–198.
- Gilaberte Y, Coscojuela C, García-Prats MD. Neutrophilic dermatosis of the dorsal hands versus pustular vasculitis. J Am Acad Dermatol. 2002;46(6):962–963.
- Mizukawa Y, Yamazaki Y, Teraki Y, et al. Direct evidence for interferon-gamma production by effector-memory-type intraepidermal T cells residing at an effector site of immunopathology in fixed drug eruption. Am J Pathol. 2002;161(4):1337–1347.
- Niebel D, Wenzel J. Immunpathologie von kutanen Medikamentennebenwirkungen. Der Pathologe. 2018;39(6):563–570.
- Suzuki S, Ho J, Rosenbaum M, Bhawan J. Neutrophilic fixed drug eruption: a mimic of neutrophilic dermatoses. Clin Exp Dermatol. 2019;44(2):236–238.
- Bisno AL, Stevens DL. Streptococcal infections of skin and soft tissues. N Engl J Med. 1996;334(4):240–245.
- Bläckberg A, Trell K, Rasmussen M. Erysipelas, a large retrospective study of aetiology and clinical presentation. BMC Infect Dis. 2015;15:402.
- Bonnetblanc J-M, Bédane C. Erysipelas: recognition and management. Am J Clin Dermatol. 2003;4(3):157–163.
- Doktor V, Hadi A, Hadi A, et al. Erythema elevatum diutinum: a case report and review of literature. Int J Dermatol. 2019;58(4):408–415.
- Micallef D, Bonnici M, Pisani D, Boffa MJ. Neutrophilic dermatosis of the dorsal hands: a review of 123 cases. J Am Acad Dermatol. 2019; S0190-9622(19)32678-7.
- Momen SE, Jorizzo J, Al-Niaimi F. Erythema elevatum diutinum: a review of presentation and treatment. J Eur Acad Dermatol Venereol. 2014;28(12):1594–1602.
- Cohen PR. Proton pump inhibitor-induced Sweet’s syndrome: report of acute febrile neutrophilic dermatosis in a woman with recurrent breast cancer. Dermatol Pract Concept. 2015;5(2):113–119.
- Mobini N, Sadrolashrafi K, Michaels S. Neutrophilic dermatosis of the dorsal hands: report of a case and review of the literature. Case Rep Dermatol Med. 2019;2019:8301585.
- Larsen HK, Danielsen AG, Krustrup D, Weismann K. Neutrophil dermatosis of the dorsal hands. J Eur Acad Dermatol Venereol. 2005;19(5): 634–637.

