The editors of JCAD are pleased to present this biannual column as a means to recognize select medical students, PhD candidates, and other young investigators in the field of dermatology for their efforts in scientific writing. We hope that the publication of their work encourages these and other emerging authors to continue their efforts in seeking new and better methods of diagnosis and treatments for patients in dermatology.
J Clin Aesthet Dermatol. 2019;12(6):55–57
 by Etuajie Oiyemhonlan, MS, BS; Carmelo Plateroti, DO, FAOCD, FAAD; and Kurt Lundquist, MD, FCAP
by Etuajie Oiyemhonlan, MS, BS; Carmelo Plateroti, DO, FAOCD, FAAD; and Kurt Lundquist, MD, FCAP
Ms. Oiyemhonlan is with the Western University of Health Sciences College of Osteopathic Medicine in Pomona, California. Dr. Plateroti is with Plateroti Dermatology in Templeton, California. Dr. Lundquist is with Western Diagnostics in Santa Maria, California.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Orofacial granulomatous (OFG) also known as granulomatous cheilitis, is a condition that causes the lips or mouth to become edematous due to a granulomatous inflammatory process. The underlying cause of the disease is unknown; however, it has been linked to other granulomatous pathologies, including sarcoidosis and Crohn’s disease. Due to the lack of evidence regarding the etiology of OFG, treatment options vary depending on the symptoms associated with the presentation of OFG and patient medical history. We present a case of long-standing idiopathic OFG in a 65-year-old African-American man. This case highlights a chronic case of OFG, associations with other disorders, the diagnostic strategy used, and management options for OFG.
KEYWORDS: Granulomatous cheilitis, angioedema, oral facial granulomatous (OFG), facial granulomatosis (FG), lip swelling, skin of color
Orofacial granulomatosis cheilitis (OFC) is an uncommon clinical disorder characterized by persistent and/or recurrent enlargement of the lips.1 Labial swelling is seen in 75.5 percent of cases of OFG.2 It is caused by a T-cell-mediated inflammatory response involving cytokines, such as tumor necrosis factor (TNF).3 The granulomas found in OFG are found in the lamina propria in association with lymphatic vessels.4 The pathogenesis of swelling is obstruction of the lymphatic drainage by granulomas.5 First described in 1985 by Leao et al,1 the clinical presentation can also include midline or angular fissuring of the lip, fissuring of the tongue, gingival enlargement, cervical lymphadenopathy, paralysis of facial nerves, and mouth ulcers. The age of onset of OFG is typically in young adulthood, having no affinity for particular ethnic backgrounds. In an analysis of more than 42 patients and 220 cases, OFG showed a predilection for women, with a mean age of 33.8 years.6 The etiology of OFG is unknown; however, it has been associated with other granulomatic diseases, such as Crohn’s disease and sarcoidosis. It has been suggested that 10 to 37 percent of patients with OFG have Crohn’s disease or oral lesions that precede intestinal involvement.7 Additionally, 54 percent of patients with endoscopic and histologic intestinal abnormalities have OFG with no gastrointestinal symptoms.8 While OFG mainly affects the labia of the mouth in 40 percent of patients, it has also been reported to be associated with facial nerve palsy (20%) and fissured tongue (40%) as part of a condition known as Melkersson-Rosenthal syndrome.9
Case Report
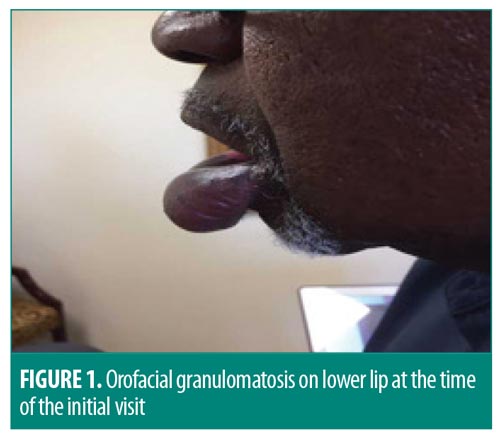
A 65-year-old African-American man presented to a dermatology office with chronic, nonpainful swelling of the lower lip present for seven years. The patient was noted to have a past medical history of anxiety, arthritis, noninsulin-dependent diabetes, hepatitis, hyperthyroidism, and prostate cancer in remission status after radiation therapy. The patient had no past childhood history of atopic dermatitis, sarcoidosis, tuberculosis, irritable bowel syndrome, or a gastrointestinal pathology such as ulcerative colitis or Crohn’s disease. Upon physical examination, the lower lip was noted to have a smooth, shiny surface in addition to being enlarged, hard, and pendulous (Figure 1). There was no facial nerve palsy, fissuring of the tongue or lip, crusting, or open wounds. Histological sections revealed lymphatic vascular ectasia with associated mixed lymphoplasmacytic inflammation and scattered, poorly formed, noncaseating granulomas against a background of dermal edema (Figure 2). Periodic acid-Schiff stain for mycosis fungoides T-cell lymphoma or Whipple disease, acid-fast bacilli stain for tuberculosis, and Fite’s stain for leprosy or norcardia returned negative. There were no vasculitidies or malignancies detected on histopathology. Chest radiography was completed to rule out active sarcoidosis or tuberculosis. Complete blood count and chemistry workup were normal.

Discussion
Differential diagnoses. OFG can be distinguished from other pathologies such as mucoceles, salivary gland tumors, caliber-persistent labial artery, and angioedema of the lips. Mucoceles present as soft, blue, asymptomatic cystic lesions and can sometimes interfere with speech and chewing.10 Our patient did not report difficulty with chewing or speech and there was diffuse lip swelling. Salivary gland tumors are almost exclusively found on the upper lip and rarely the lower lip.11 Caliber-persistent labial artery is a vascular tumor that presents as a pulsatile elevation of lip; this was not characteristic of the lesion seen on our patient.12 Hereditary angioedema typically develops during childhood and is characterized by recurrent episodes of severe swelling that can develop on the limbs, face, gastrointestinal tract, and airway.13 Episodes can present with shortness of breath, vomiting, abdominal pain, and nausea. However, this did not correspond with the history reported by our patient.
Diagnostic methods. The diagnosis of OFG is via lesional biopsy and treatment consists of lifestyle changes relating to diet if it is associated with irritable bowel syndrome; topical or systematic steroids for swelling; and immune modulators such as azathioprine, methotrexate, and TNF-alpha inhibitors, such as infliximab. Surgery can be beneficial for severe permanent swelling.9
Treatment. Our patient had an extensive medical history, so we had to risk stratify many of our treatment options. There have been prior studies that showed successful treatment of OFG with intralesional triamcinolone; however, this requires repeated future injections to prevent reccurrence.14,15 Intralesional steroid injections with triamcinolone can be contraindicated in diabetics and individuals with psychiatric illness.14 Clofazamine, an oral phenazine dye used in leprosy, has also been used to treat OFG. Clofazamine has antibacterial, anti-inflammatory, and immunomodulatory properties that can be useful in conditions characterized by granulomas.15 The TNF-alpha inhibitor infliximab has been used in patients with OFG and Crohn’s disease, but topical immune modulators like clofazamine and infliximab can also be challenging to use in individuals with a history of malignancy postradiation therapy.15 Kruse-Losler et al16 showed that reduction cheiloplasty could be used to manage OFG in individuals with a persistent state of the disease.16
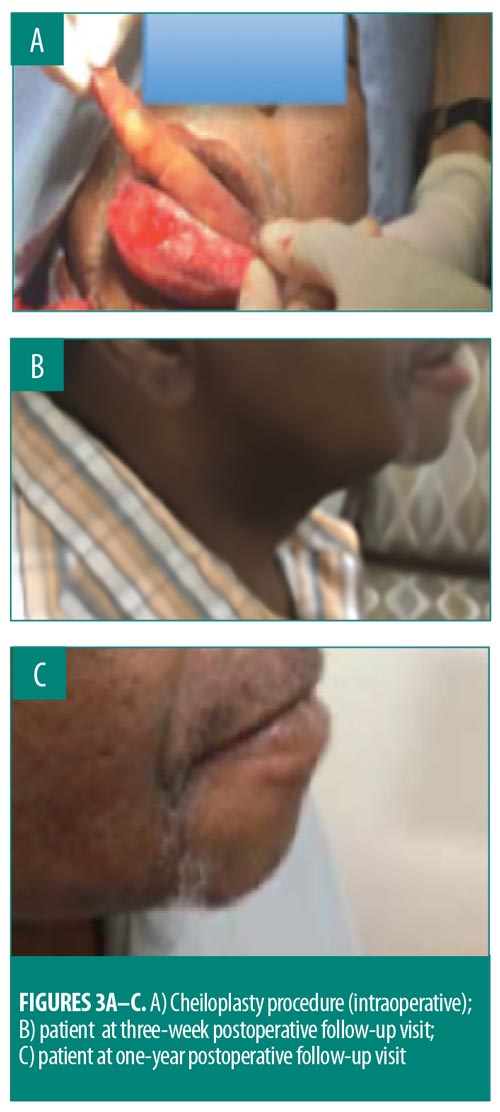
Given our patient’s medical history, surgery was required to provide the best clinical outcome, which involved a lower cheiloplasty under local anesthesia. A large, full-thickness wedge of tissue was removed, maintaining an incision on the inner aspect of the lip (Figure 3A). Sutures were removed on Day 7. At the three-week postoperative follow-up visit, the swelling had resolved and the patient reported improvement in the appearance of his lower lip and increased self-confidence (Figure 3B). At the one-year postoperative follow-up visit, the patient appeared to be doing well, with no recurrence of the granulomatous cheilitis (Figure 3C).
Conclusion
OFG is a rare, inflammatory, granulomatous disease. The exact etiology is not clear, though there have been links with other inflammatory and granulomatous conditions, including tuberculosis, sarcoidosis, and Crohn’s disease. Because the etiology is still unclear, the ideal treatment and long-term prognosis of OFG is also unknown. Treatment options range from lifestyle management to surgical intervention. Due to the varying associations and treatments, a clinician should have an understanding of the clinical history and features of this condition so as to provide treatment options to the patient based on medical history.
Acknowledgments
The authors wish to acknowledge Sebastian Fuchs MD, PhD, of the Department of Biomedical Sciences, Western University of Health Sciences College of Osteopathic Medicine in Pomona, California.
References
- Leao JC, Hodgson T, Scully C, Porter S. Review article: orofacial granulomatosis. Aliment Pharmacol Ther. 2004;20(10):1019–1027.
- Al Johani KA, Moles DR, Hodgson TA, et al. Orofacial granulomatosis: clinical features and long-term outcome of therapy. J Am Acad Dermatol. 2010;62(4):611–620.
- Scully CA. Oral and Maxillofacial Medicine: The Basis of Diagnosis and Treatment. 3rd ed. Edinburgh, NY: Churchill Livingstone/Elsevier; 2013.
- Marcoval J, Penin RM. Histopathological features of orofacial granulomatosis. Am J Dermatopathol. 2016;38(3):194–200.
- Savas J, Sokoloff D, Sanchez KM, Lichtstein DM. Granulomatous cheilitis: a stiff upper lip. Cutis. 2015;96(3):E18–E20.
- Zimmer WM, Rogers RS 3rd, Reeve CM, Sheridan PJ. Orofacial manifestations of Melkersson-Rosenthal syndrome. A study of 42 patients and review of 220 cases from the literature. Oral Surg Oral Med Oral Pathol. 1992;74(5):610–619.
- Bishop RP, Brewster AC, Antonioli DA. Crohn’s disease of the mouth. Gastroenterology. 1972;62(2):302–306.
- Sanderson J, Nunes C, Escudier M, et al. Oro-facial granulomatosis: Crohn’s disease or a new inflammatory bowel disease?. Inflamm Bowel Dis. 2005;11(9):840–846.
- Worsaae N, Christensen KC, Schiodt M, Reibel J. Melkersson–Rosenthal syndrome and cheilitis granulomatosa. A clinicopathological study of thirty-three patients with special reference to their oral lesions. Oral Surg Oral Med Oral Pathol. 1982;54(4):404–413.
- Chaitanya P, Praveen D, Reddy M. Mucocele on lower lip: a case series. Indian Dermatol Online J. 2017;8(3):205–207.
- Speight PM, Barrett AW. Salivary gland tumours. Oral Dis. 2002;8(5):229–240.
- Rosdy NM, Firth NA, Rich AM. Calibre-persistent labial artery: often misdiagnosed as a mucocoele. Int J Oral Maxillofac Surg. 2010;39(12):1230–1233.
- Banerji A. Hereditary angioedema: classification, pathogenesis, and diagnosis. Allergy Asthma Proc. 2011;32(6):403–407.
- Rangdhol RV, Madhulika N, Dany A, et al. Idiopathic orofacial granulomatosis-a diagnostic and treatment challenge. J Clin Diagn Res. 2014;8(11):ZD07–ZD10.
- Fdez-Freire LR, Serrano Gotarredona A, Bernabeu Wittel J, et al. Clofazimine as elective treatment for granulomatous cheilitis. J Drugs Dermatol. 2005;4(3):374–377.
- Kruse-Losler B, Presser D, Metze D, Joos U. Surgical treatment of persistent macrocheilia in patients with Melkersson–Rosenthal syndrome and cheilitis granulomatosa. Arch Dermatol. 2005;141(9):1085–1091.

