 J Clin Aesthet Dermatol. 2022;15(3):38–43.
J Clin Aesthet Dermatol. 2022;15(3):38–43.
by Irina Aksenenko, PhD; Marina Gerasimenko, MD; Viktoria Polunina, PhD
and Inna Evstigneeva, PhD
Drs. Aksenenko, Gerasimenko, and Evstigneeva are with the Federal State Budgetary Educational Institution of Further Professional Education of the Ministry of Healthcare of the Russian Federation in Moscow, Russia. Dr. Polunina is with the Pirogov Russian National Research Medical University in Moscow, Russia.
ABSTRACT: Background. Fillers based on calcium hydroxyapatite (CaHA) have become popular for the correction of involutive skin changes. However, if the filler injection technique is violated, undesirable events can occur in the skin, the treatment of which is complicated by the lack of a specific antidote to CaHA.
Objective. In this study, we aimed to evaluate the effectiveness of a combined method that includes a course of ultraphonophoresis of collagenase and diadynamophoresis of sodium thiosulfate (Na2S2O3) for the treatment of complications developed after contour correction with CaHA-based fillers.
Methods. The study included 37 women aged 47.2±5.9 years old with a complication developed after the superficial injection of a CaHA-based filler localized in the facial area. The patients were divided into three groups; Group I received a course of ultraphonophoresis of collagenase (Collalysin 1000 CU); Group II received a course of diadynamophoresis of 30% Na2S2O3; and Group III received a combined treatment.
Results. A combined course (Group III) had a significant effect expressed as a reduction of contouration, gel visualization, local edema, and neuropathy, as well as a stabilized psychoemotional condition of patients. This treatment complex significantly accelerates the biodegradation of the filler and exerts a restructuring effect.
Conclusion. The application of this combined treatment course in patients with complications following the superficial injection of CaHA-based filler appears to be a highly effective treatment method, which was confirmed by the resolution of clinical symptoms, accelerated drug biodegradation, and an increase in the patients’ quality of life.
Keywords. Collagenase, calcium hydroxyapatite (CaHA), neuropathy, diadynamophoresis, sodium thiosulfate (Na2S2O3), complications
Fillers based on calcium hydroxyapatite (CaHA) for subcutaneous injection have become very popular for the correction of involutive skin changes. They are used not only to fill wrinkles and skin folds but also to stimulate the expression of collagen types I and III.1–5 To stimulate collagen expression and correct involutive changes of the skin with decreased tonus of the facial and body skin, it is recommended to inject the drug in different concentrations and more superficially, subdermally, which requires thorough attention and compliance with the guidelines on the injection level of this drug.6–9 However, the widespread use of this method has a reverse side associated with the lack of a specific antidote and impossibility to “dissolve” the drug quickly and accelerate the biodegradation of CaHA in the case of adverse effects. For example, it can be observed in the case of injection of the drug too high in the skin surface or injection of an excessive amount in the skin. The effect of the drug lasts up to 12 months, on average, according to the manufacturer.
One of the most frequent complications that specialists face in their practice is a superficial injection of the filler based on CaHA: intradermal or subcutaneous, especially in patients with thin skin. It is manifested as contouration, gel visualization, local skin induration, or changes in the skin color (whitish color) due to visualization of white CaHA crystals. In the case of early diagnostics of hypercorrection of the filler (2–3 weeks after superficially injected CaHA-based filler), good results are obtained by the method of “washing out”, i.e., injection of a saline solution and massage of the drug consolidation area, which provides even distribution of the drug in the skin.10 However, in the case of late diagnostics, massage is not sufficient for the distribution of the drug. This is associated with the simulating effect of CaHA granules on fibroblasts and the production of the pool of collagen fibers that compress the surrounding tissues when adhering to the superficially injected filler. Such a complication is hard to correct and worsens the quality of life of patients. To correct such adverse events as cicatricle changes in the skin and to accelerate biodegradation of the superficially injected filler due to the enhancement of intra-tissue processes, including hydrolysis, it is recommended to use such physiotherapeutic methods as low-intensive laser therapy, vacuum massage, darsonvalization, carboxytherapy, and fractional CO2 lasers.11
To correct cicatricle processes in the skin, proteolytic enzymes are used as injections12 and different physiotherapeutic methods of introduction.13 Collagenase is one of the most effective proteolytic enzymes because it is capable of splitting peptide bonds in collagen, which is the main component of wound healing and cicatrix formation.14 “Collalysin” (INN “Collagenase”) is registered in the State Register of Medicines of the RF, LSR-005615/09: a proteolytic enzyme that exerts a keloid-lytic effect; produced in the form of lyophilizate powder at a dose of 100–1000 CU for the preparation of the solution for injections and electrophoresis for the treatment of burns and correction of cicatrices.15 Collagenase can be introduced into the skin by non-invasive methods, like phonophoresis or electrophoresis.16,17
The advantage of diadynamophoresis in comparison with electrophoresis is in a more diverse effect on the organism (analgesic, trophic, and dissolving). The introduction of collagenase using diadynamophoresis is more preferable than injections because of the noninvasiveness of the method, more convenient and mild gradual application on especially sensitive areas, and the possibility of deep introduction on a vast area of the pathologic process.
Sodium thiosulfate is known to exert different effects on the organism, in particular, detoxifying, anti-inflammatory, desensitizing, and is used as an antidote to numerous heavy metals. It is widely used as a part of complex therapy for different diseases, in particular, neuralgias. There were cases of successful treatment of different calcifications, including cutaneous, using sodium thiosulfate.18–22 However, after the injection of the drug into the area of the calcified nodule, expressed local reactions manifested as edema and hyperemia were observed. The advantage of the physiotherapeutic method of introduction of sodium thiosulfate is the high concentration of the drug in the introduction foci. When the substance dissociates into ions under electric current, it exerts a higher activity in comparison with a molecular form. The treatment requires less amount of a drug, which decreases the total pharmaceutical load on the organism.
Clinical manifestations (e.g., contouration, local skin induration) observed in patients with such complications as the superficial injection of a CaHA-based filler in the facial skin develop because of compression of tissues by a conglomerate made of filler fragments and fibrotic tissues. The compression can be enhanced due to the production of collagen stimulated by the crystals of the drug. As a result, local edema develops that is associated with the moderate manifestation of neuropathy. In general, these factors have a significant psychological effect on patients. The application of electrophoresis of sodium thiosulfate for the reduction of the reactivity of the surrounding tissues, edema, and neuropathic manifestations together with diadynamophoresis of collagenase not only to affect pathologically produced collagen but also to reduce edema and neuropathy is a feasible combined method for the treatment of adverse events and complications after superficially injected CaHA-based fillers in cosmetology, which significantly improves the aesthetic profile, psychological status, and quality of life of patients. Thus, the present study aimed to evaluate the effectiveness of a combined method that included a course of ultraphonophoresis of collagenase (Collalysin 1000 CU) and diadynamophoresis of 30% sodium thiosulfate for the resolution of complications developed after facial contour correction with CaHA-based fillers.
Methods
The study included 37 women aged 47.2±5.9 years old who were referred to the Clinics of Esthetical Medicine LLC from 2017 to 2020 from third-party organizations after a procedure of contour correction with a CaHA-based filler with a complication: a visualized light focus of skin induration after superficial injection of the filler localized in the facial area (buccal and malar areas). All patients had a single area of different sizes (0.5–1cm in diameter) of altered skin.
The anamnesis showed that all patients had undergone contour correction in the facial area to improve the skin tonus with a CaHA-based drug 1.5 to 2 months earlier. After the procedure, short-term moderate edema and painfulness developed; single hematomas appeared several days later. During the recreation period, the majority of patients applied the Traumeel® (Biologische Heilmittel Heel GmbH, Baden-Baden, Germany) ointment topically and took antihistamine and diuretic drugs if it was necessary within the first days after the procedure. Right after the procedure, a small focus of skin induration and color change (whitish color) appeared that was slightly painful during palpation. Occasionally, patients experienced mild paresthesia or hypoesthesia of the skin in the focus of induration. According to the treating doctors’ recommendations, the patients underwent massage and the procedure of “washing out” of the hypercorrection focus with a saline solution. These measures improved the condition but the induration area did not regress. In all the patients, the ultrasonic investigation revealed a single hyperechogenic focus adjoining the dermal-hypodermal border. The epidermis was exhausted; the derma was deformed, and its thickness was significantly increased. The hypodermal border was smoothed. All patients underwent the procedure of diadynamophoresis of sodium thiosulfate with an apparatus Mustang-Physio-MELT-2K (RU No. FSR 2008/03578 dated October 31, 2010) (a course of 10 procedures) and (or) a course of ultraphonophoresis of collagenase (Collalisin 1000 CU) with an apparatus UZT-101 (RU No. FSR 2012/13549 dated June 22, 2012, no expiration date). Patients who underwent combined therapy received diadynamophoresis of 5% of sodium thiosulfate first, and then, ultraphonophoresis of collagenase.
Patients were randomly divided into three groups. Patients in Group I (n=12) received only ultraphonophoresis of collagenase (Collalisin 1000 CU) in a course of 10 procedures. Patients in Group II (n=12) received only diadynamophoresis of sodium thiosulfate in a course of 10 procedures. Patients in Group III (n=13) received a combined therapy consisting of a course of diadynamophoresis of sodium thiosulfate and ultraphonophoresis of collagenase in one day, daily, a course of 10 procedures.
The duration of therapy in each group was 10 days.
The following studies were conducted for the objective evaluation of the patients’ condition and dynamics. The analysis of the symptoms of phobic anxiety disorders, including the factors of trait anxiety (TA) and state anxiety (SA) that affect adaptation, was performed using Spielberg’s test (STAI). The results were interpreted as follows: up to 30 points (mild anxiety), 31–45 points (moderate anxiety), 46 points and more (severe anxiety). Additional evaluation of the psychological status was performed using the WAM inventory (well-being, activity, mood). The evaluation of the parameters was made before the treatment and one and three months after the treatment.
Ultrasonic sonography was used to examine the echostructural peculiarities of the epidermis, derma, and hypodermis (Dub Cutis 22-75, TPM, Germany, sensor 22 MHz, registration certificate No. RZN 2016/5165 dated April 26, 2017, no expiration date). The thickness of the epidermis and derma and the coefficient of dermal density were evaluated, which indirectly reflected the intensity of the dermal edema. The dynamics of filler biodegradation were observed in each group by the mean volume of CaHA superficially injected into the skin. The patients were examined before treatment and one and three months after the treatment.
The observation period was three months after the beginning of the treatment.
The method of diadynamophoresis of sodium thiosulfate: a 30% solution of sodium thiosulfate was introduced with a cathode. The electrode was placed on the hypercorrection focus on one side of the face. The cathode was placed on the same side in the area of the mastoid process. Two-stroke continuous current was used for two minutes, followed by a short current period of up to 10 minutes. The course included 10 procedures, daily.
The method of ultraphonoresis of collagenase (Collalisin 1000 CU): Collalysin 1000 CU was diluted in 2–3 mL of gel for ultrasound therapy (Repack-T), which was placed on the pathological focus. The affected part of the face was treated in the induration area. The intensity was 0.2–0.4 W/cm2, the mode of operation was continuous, the application method was labile. The duration of the procedure was 5–8 minutes, daily. The course consisted of 10 procedures. The procedures were tolerated well. All statistical calculations were performed using Statistica for Windows 10 (Statsoft).
Results
The results of Spielberg’s tests and the WAM inventory, as the most informative method of self-evaluation of the levels of SA, TA, and psychological status, respectively, showed positive dynamics in all the studied groups.
Before the treatment, Spielberg’s test score was high. However, in the main group, the stabilization of the psychological status and a decrease in the SA and TA scores to the level of “mild anxiety” were observed already during the 1st month of observation. In the groups of comparison, the levels of SA and TA scores had a positive tendency but still were evaluated as “moderate anxiety”, and the normalization of these parameters was registered only three months later. These changes correlated with the results of WAM testing. Positive changes in the patients’ psychoemotional status were observed in all the groups. However, one month after the start of the treatment, even though the summed score of the WAM inventory in both groups of comparison had a positive tendency in comparison with the baseline values in the respective groups, there were no statistically significant changes revealed in these groups. At the same time, in the main group, an increase in the WAM index was statistically significant already during the first month of the observation, which determined the aim of the therapy in patients with complications developed after a superficial injection of the filler as an increase in the patients’ quality of life as early as possible after the adverse event (Table 1).
The pathological process was evaluated, in particular, by such parameters as the thickness of the epidermis and derma, the coefficient of dermal density, as well as the dynamics of biodegradation of the superficially injected drug (a decrease in the volume of the earlier injected filled). The latter parameter was especially informative and was visualized due to a significant difference in the echo-response from the CaHA-based filler and skin tissues. Ultrasonic investigation showed that the depth of pathological focus (superficially injected filler) in the site of its contouration was not more than 0.5mm.
The thickness of the epidermis in the studied groups increased after the therapy on the 1st and 3rd months of the observation and did not differ significantly from the respective parameters in all the groups. During the first month, the thickness of the derma reduced by 14.4 percent in comparison with Groups of comparison I and II, wherein this parameter decreased by 6.1 percent and 7.2 percent, respectively. Three months later, in the main group, this parameter decreased by 16.8 percent in comparison with Groups of comparison I and II, wherein this parameter decreased by 7.5 percent and 7.6 percent, respectively.
In the main group, the coefficient of the ultrasound density of the derma increased by 12.5 percent, while in Groups of comparison I and II, it increased only by 5.9 percent and 6.3 percent, respectively. Three months later, in the main group, the studied parameter increased by 16.1 percent, while in Groups of comparison I and II, the coefficient of ultrasonic density increased insignificantly by 6.8 percent and 7.1 percent, respectively. It should be mentioned that the improvement of the ultrasonic picture and a significant reduction of the signs of intradermal edema in the main group were especially evident in the early period of observation (a month after the beginning of the treatment). These data indirectly indicate a faster reduction (by more than 2 times) of intradermal edema in the early period of observation in the main group in comparison with both groups of comparison.
This combined method of treatment significantly accelerates the biodegradation of superficially injected filler in the pathological focus. The volume of superficially injected and contoured filler in the main group reduced by 2.27 times one month later and by 3.81 times 3 months later in comparison with the parameters in Group of comparison I (by 1.38 and 2.16 times) and Group of comparison II (by 1.48 and 2.72 times, respectively). This significantly reduced the recovery period in the main group in comparison with the groups of comparison. It should be noted that in the patients in the group of comparison that underwent diadynamophoresis of sodium thiosulfate, biodegradation of the CaHA-based drug was more significant than in the Group of comparison I in the 1st and 3rd month of the observation. There is no scientific evidence that could explain this fact. It is suggested that sodium thiosulfate is an indirect antidote to calcium hydroxyapatite, which requires further studies on the interaction and effect of this combination (Table 2).
After the course of treatment in the main group, contouration and skin induration were not visible by the 1st month of the observation. In the groups of comparison, clinical improvement was also observed (contouration and induration reduced, local skin color changed). These visual signs were resolved only by the 3rd month of the observation.
During the period of observation, no edemas were registered in the patients. Thus, the authors can recommend a combined application of ultraphonophoresis of collagenase (Collalysin 1000 CU) and diadynamophoresis of sodium thiosulfate of a 5% solution of sodium thiosulfate as a course that exerts a synergic effect for the resolution of late complications that develop after contour correction of the face with CaHA-based fillers. This combined approach significantly reduces the time of recovery and improves the patients’ psychological state and esthetical profile, which increases their quality of life.
Clinical case. Patient V was a 39-year-old female patient who received an injection of a calcium hydroxylapatite filler in the malar region two months prior to visiting our clinic. A whitish area of 0.9mm was visualized in the left malar region. The area was dense and elevated above the skin level, painless at palpation (Figure 1A). Light hypoesthesia was observed in the focus of the altered skin. A course of diadynamophoresis of sodium thiosulfate combined with a course of ultraphonophoresis of collagenase on the same day (daily, 10 procedures) was performed.

A month after the beginning of treatment, the whitish area was not visualized. The signs of hypoesthesia resolved (Figure 2b).
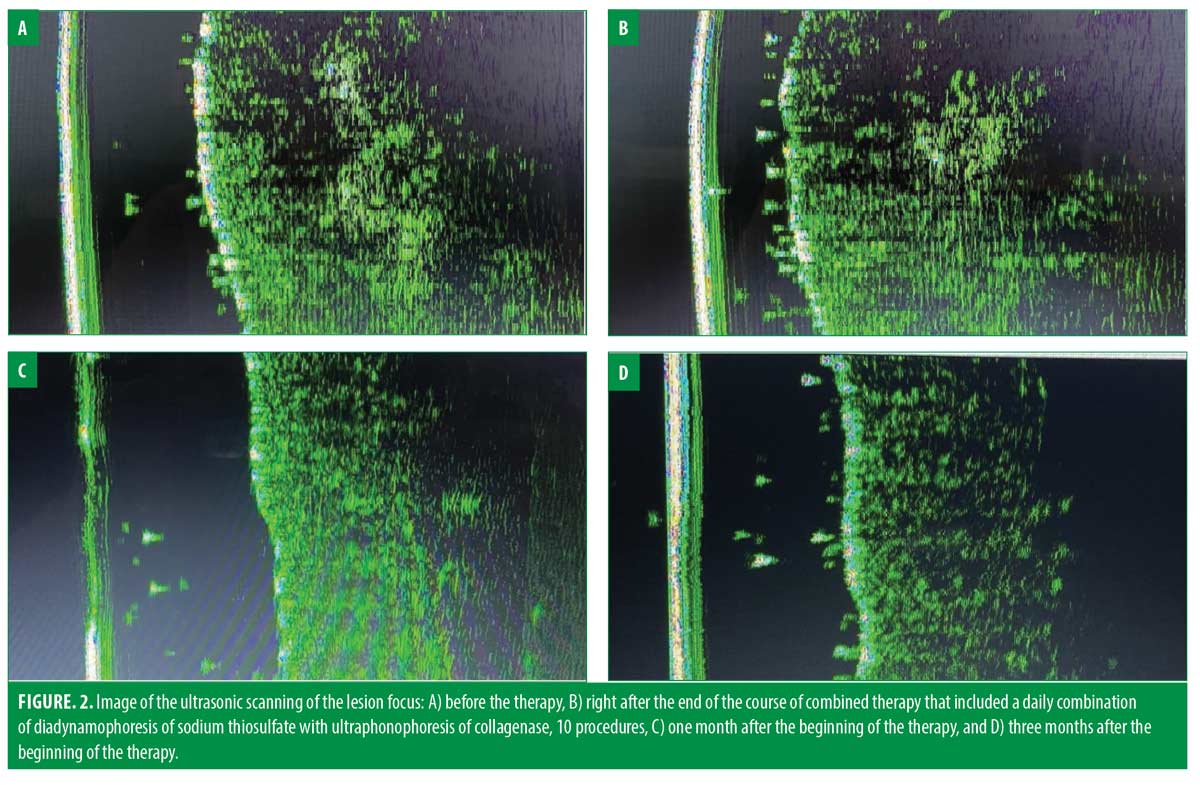
Ultrasonic investigation of the skin revealed a focus of increased echogenicity. The volume of superficially injected filler was 0.892 cm.2 Moderate dermal and hypodermal edema was observed.
After the end of the course of therapy, the volume of superficially injected filler reduced by 1.8 times in the focus of lesion; one month after the beginning of the therapy – by 2.2 times, and three months after the beginning of the therapy – by 3.85 times. The signs of edema regressed.
Conclusion
Though the injections of CaHA-based fillers have become more and more widespread as a method of low-invasive skin resurfacing, clinicians should be aware that the failure to comply with the guidelines and the technology of the procedure can lead to complications and adverse events like the superficial injection of the drug, which is characterized by contouration, filler visualization, local edema, and neuropathy. Their correction is complicated by the lack of a specific antidote for CaHA. Based on our study results, a combined course of ultraphonophoresis of collagenase (Collalisin 1000 CU) and diadynamophoresis of sodium thiosulfate applied locally to the pathological focus is a highly effective method of treatment for complications that develop after the superficial injection of CaHA-based filler. This method accelerates the biodegradation of the drug, resolves early clinical symptoms, and improves the quality of life of patients.
References
- Berlin A., Cohen J.L., Goldberg D.J. Calcium hydroxylapatite for facial rejuvenation. Seminars in Cutaneous Medicine and Surgery 2006; 25(3): 132-137
- Marmur E.S., Phelps R., Goldberg D.J. Clinical, histologic and electron microscopic findings after injection of a calcium hydroxylapatite filler. Journal of Cosmetic and Laser Therapy 2004; 6(4): 223-226
- Yutskovskaya Y.A., Kogan E.A. Improved neocollagenesis and skin mechanical properties after injection of diluted calcium hydroxylapatite in the neck and décolletage: a pilot study. Journal of Drugs in Dermatology 2017; 16(1): 68-74.
- Goldie K., Peeters W., Alghoul M., Butterwick K., Casabona G., Yen Y., Chao Y., Costa J., Eviatar J., Fabi S.G., Lupo M., Sattler G., Waldorf H., Yutskovskaya Y., Lorenc P. Global Consensus Guidelines for the Injection of Diluted and Hyperdiluted Calcium Hydroxylapatite for Skin Tightening. Dermatologic Surgery 2018; 44: 32-41
- Rovatti P.P., Pellacani G., Guida S. Hyperdiluted Calcium Hydroxylapatite. Dermatologic Surgery 2020; 1
- Lapatina N.G., Pavlenko T. Diluted calcium hydroxylapatite for skin tightening of the upper arms and abdomen. Journal of Drugs in Dermatology 2017; 16 (9): 900-906
- Chao Y.Y., Chiu H.H, Howell D.J. A novel injection technique for horizontal neck lines correction using calcium hydroxylapatite. Dermatologic Surgery 2011; 37(10): 1542-1545
- Amselem M. Radiesse: a novel rejuvenation treatment for the upper arms. Clinical, Cosmetic and Investigational Dermatology 2015; 9(1): 9-14
- Chao Y.Y., Kim J.W., Kim J., Ko H., Goldie K. Hyperdilution of CaHA fillers for the improvement of age and hereditary volume deficits in East Asian patients. Clinical Cosmetic and Investigational Dermatology 2018; 11: 357-363
- Voigts R., Devore D.P., Grazer J.M. Dispersion of Calcium Hydroxylapatite accumulations in the skin. Dermatologic Surgery 2010; 36 (1): 798-803,
- Reddy K.K., Brauer J.A., Anolik R., Bernstein L., Brightman L.A., Hale E., Karen J., Weiss E., Geronemus R.G. Calcium hydroxylapatite nodule resolution after fractional carbon dioxid laser therapy. Archives of Dermatology 2012; 148 (5): 634-636
- Paramonov B. A. Collagenolytic enzymes Part 2. Use for cleaning wounds. Cosmetics and medicine 2016; 2: 38-48.
- Gerasimenko M.Y., Aksenenko I.P. Combined use of fractional CO2 laser and diadinamophoresis collalizin in the correction of complications contouring. Physiotherapy, balneology and rehabilitation 2018, 17 (5): 254-257.
- Paramonov B.A. Collagenolytic enzymes. Unsolved and controversial issues of theory and practice. Cosmetics and medicine 2016; 1: 32-41.
- Trunin E. M., Kandalova I. G., Now I. V., Berestova L. K., Obrazkova A.V. The Use of Collisin for the treatment of hypertrophic scars after thyroid surgery 2009; 1: 120-121.
- Peresadina S.K., Vasin A.S. Application of phonophoresis gel Fermenkol in the treatment of pitted acne scars. Dermatology in Russia, 2017; S1:75-76
- Mayorova A.V., Sysuev B.B., Ivankova J.O., Hanalieva I.A. Collagenases in medical practice: modern collagenase-based preparations and prospects for their improvement. Pharmacy & Pharmacology 2019; 7(5): 260-270,
- Rullan P.P., Olson R., Lee K.C. The use of intralesional sodium thiosulfate to dissolve facial nodules from calcium hydroxylapatite. Dermatologic Surgery, 2019; 1
- Strazzula L., Nigwekar S.U., Steele D., Tsiaras W., Sise M.E, Bis S., Smith G.P., Kroshinsky D. Intralesional sodium thiosulfate for the treatment of calciphylaxis. JAMA Dermatology, 2013; 149(8): 946-949,
- Hayden M.R., Goldsmith D.J. Sodium thiosulfate: new hope for the treatment of calciphylaxis. Semin Dial. 2010; 23(3): 258-262.
- Musso C.G., Enz P., Vidal F., et al. Use of sodium thiosulfate in the treatment of calciphylaxis. Saudi J Kidney Dis Transpl, 2009; 20(6): 1065-1068.
- Auriemma M., Carbone A., Lorenzo Di Liberato, Cupaiolo A., Chiara Caponio, Clara De Simone, Tulli A., Bonomini M., Amerio P. Treatment of cutaneous calciphylaxis with sodium thiosulfate: two case reports and a review of the literature. Am J Clin Dermatol, 2011; 12(5): 339-46

